Allergies are becoming one of the most common medical problems people face. Allergies are a hot issue every year, starting at the very least with the beginning of hay fever season, and not only among people who suffer from them. It is hypothesized that allergies are on the rise, that they are the “scourge of the industrial age,” and that the environment is to blame. Is there any truth to these rumors? Is there actually an increasing number of people with allergies, or have both physicians and patients grown more aware of the issue? Where do allergens come from? Why do some individuals have allergic reactions and others do not, and what is really happening in the body? What properties do allergens have that set them apart from other substances?
- Allergies on the rise
- Is it an allergy or a common cold?
- When an allergy is not an allergy at all
- The four allergy types
- Who gets an allergy?
- Genes or environment?
- What makes a substance an allergen?
- Analyzing an allergic reaction from an immunological standpoint
- The immune system’s protective cells
- Humoral immune defense and antibodies
Allergies on the rise
Attacking the alleged antagonist
Most individuals would feel happy and contented if they were surrounded by flowering meadows and trees, their beloved pet, and a large dish of strawberries covered in whipped cream. However, these substances may trigger allergic reactions in some individuals, including sneezing, wheezing, or a rash.
In the meantime, allergies have almost reached pandemic proportions; one in four people in developed countries suffers from them. In those countries, hay fever is the most prevalent and well-known kind of allergy, affecting an estimated 10 million individuals on average. Allergists currently estimate that 35 percent of youngsters suffer from allergies, and studies suggest that this trend is most noticeable in younger age groups.
Scientists are still trying to figure out what is causing allergies to spread like wildfire in the modern industrial era. The irony here is that the “primary culprit” does not seem to be environmental contamination; rather, specialists increasingly prefer to consider the “blessings” of contemporary life as the source of sickness.
Our children are increasingly growing up in overprotected homes. Children do not have naturally developed immune systems; rather, they must learn to use their bodies’ natural mechanisms to fight off infections. We live in a society where childhood infections are becoming rare. However, they pose a significant problem for the immune system.
The immune system develops the ability to tell the difference between “foreign and dangerous” and “foreign and innocuous” throughout infancy. The body’s “protective soldiers” are normally “whistled back” when they come into contact with innocuous substances, but control systems guarantee that infections like bacteria or viruses are battled. In those who have allergies, the immune system mistakes harmless things like pollen and dust for dangerous invaders and launches an offensive against them. Allergy patients are familiar with the symptoms that follow an allergic reaction: congestion, itching, redness, and watery eyes or nose.
When the immune system overreacts in this way to otherwise benign chemicals, we speak of a “real” allergy. Allergies almost seldom manifest at the first interaction with a given allergen but rather develop with repeated exposure. Until then, the allergen is not recognized as an adversary, and hence no defensive mechanism is activated.
Is it an allergy or a common cold?
Common allergy signs and symptoms
Is that bothersome cold an actual illness, or just a reaction to pollen in the air? Is it possible for an allergy to cause a headache? While only an allergy test and a doctor’s visit can confirm whether or not you have an allergy, experiencing more than one of the symptoms listed below at the same time may be cause for concern: Reddened, watery and swollen eyes in combination with a runny or stuffy nose and frequent sneezing without fever, body aches or other clear cold symptoms.
You can also pay close attention to the times when the symptoms are most severe: Symptoms of hay fever often intensify while outdoors or in the evening, whereas those of a home dust allergy typically worsen at night and upon waking up.
A trip to the doctor is in order if the “sniffles” remain for more than a few weeks, or if you have persistent coughing or shortness of breath that doesn’t seem to be related to a cold.
It’s possible that you have a food intolerance if you often experience symptoms like nausea and stomach pain after consuming the offending item. It’s possible that your coffee or chocolate headache is really an allergic reaction.
Acne, hives, and other skin reactions including redness, swelling, and weeping or itching are not always the result of an allergic response.
These or similar symptoms should prompt a visit to the doctor, and maybe an allergy test, especially if one or both sets of parents or grandparents also have allergies.
When an allergy is not an allergy at all
Hyposensitivity and other exaggerated responses
A food allergy would cause severe itching, redness, and blistering of the skin only hours after consuming milk, strawberries, or tuna. Food allergies, a topic of heated debate in the medical community, seem to be on the rise in the modern world. Meal allergies are blamed for anything from hives and diarrhea to depression and schizophrenia, and it seems that there is barely a food that can be considered “guilt-free.”
Is an allergy always the cause? If not allergies, then what else may trigger such reactions? Allergies are defined as a reaction to an allergen that is overreacted to by the immune system, whereas intolerances and pseudo-allergies induce similar symptoms but are caused by a different mechanism.
In many cases, what people label as “food allergies” are really intolerance responses rather than true allergic reactions. A questionnaire campaign was conducted in Switzerland by allergists to learn more about how food allergies affect individuals there. 12 to 18 percent of respondents indicated they had food intolerances, despite European specialists estimating the frequency of allergies in adults at approximately one to two percent.
The phrase “allergic to milk” is used to describe the condition in which certain children have problems from birth. Cow’s milk causes severe diarrhea and, in the worst situations, may cause a baby to die from a lack of oxygen to the brain. It turns out that this is an intolerance rather than an allergy. A lack of lactase, an enzyme necessary for milk digestion, is to blame. The milk’s lactose cannot be digested without this lactase, therefore the body must find other methods to get rid of it.
However, the unpleasant effects of intolerances might still occur even if you have a “full” enzyme arsenal. Pseudoallergic responses, for instance, have been shown to impact almost everyone. In this scenario, the “villains” are identified as individual components of certain meals and medicines: Histamine is a mediator chemical that is present in certain foods (like cheese, sauerkraut, and strawberries) or that stimulates the production of histamine in some mucosal cells (like contrast media used in X-ray exams and antispasmodic medicines). This chemical, which is also implicated in allergic responses, then acts directly on mucous membranes and blood vessels, causing swelling of the mucous membranes, skin rashes, and/or headaches in sensitive people.
Histamine is the culprit in certain cases of “fish allergy,” since it is commonly produced by bacteria found in preserved tuna and mackerel. Aspirin intolerance has been recognized as a classic example of a drug allergy since its discovery at the turn of the century. Examples of this intolerance, including asthma episodes, skin rashes, and mucosal swelling, were detailed in a 1919 paper.
Unfortunately, more and more data suggests that this case in point is not representative: the purported allergy is most likely the result of a hypersensitive response to salicylic acid. Whether or not intolerance is really an allergy is an important subject, particularly from a therapeutic standpoint. While hyposensitization is typically a long-term solution for those who suffer from allergic reactions, such “habituation treatment” would be ineffective at best and may be harmful in the cases of intolerance and pseudoallergy.
The four allergy types
Not all allergies are the same
Allergic responses may take on an almost infinite variety of looks and characteristics. There are innumerable “exotic” intolerances, such as Farmer’s lung and Lyell’s syndrome, in addition to “ordinary” allergens like hay fever and asthma. This overabundance motivated British allergists Robin Coombs and Philip Gell to “establish order” as early as the 1960s.
This led to the creation of the now-standard four-category system: Immediate-type allergies fall within the first three groups. Allergies are similar in that they cause symptoms within a few hours of exposure to the offending allergen. Anaphylaxis is a potentially fatal reaction to an allergen that may develop within seconds of first exposure. In most cases, IgE antibodies are to blame for all three forms of allergy symptoms.
Type 1 allergy
The IgE antibodies that are “stationed” in mast cells play a crucial role in type 1 allergies. They trigger the release of mediators in response to allergen contact, which in turn causes an acute reaction (e.g., swelling of the mucous membranes, constriction of the bronchial passages, or the formation of wheals on the skin). When shock symptoms and circulatory failure are coupled with an allergic reaction, the result is anaphylactic shock. Examples of this category of allergens include hay fever, asthma, and neurodermatitis.
Type 2 allergy
The damaging impact on cells is characteristic of type 2 allergies. Allergens, antibodies, and other immune system chemicals bind to cells throughout the body. The free-eating and killer cells drawn to it designate the cell as “cleared for firing,” destroying it. These allergic responses may lead to anemia and problems with blood clotting since they primarily impact red blood cells. Allergens are often medications like penicillin.
Type 3 allergy
Type 3 allergies are caused by an immunological complex consisting of an allergen and an antibody. After floating about in the blood for a while, it eventually affixes to the inside of the blood vessels. Attracted white blood cells secrete enzymes that set off inflammation at the location. Inflammation of the kidneys, blood arteries, or inner heart walls may accompany fever and joint discomfort. Farmer’s lung is an allergy to mold spores in the hay; serum sickness was a result of injecting exogenous blood serum, and passive immunizations often caused infections.
Type 4 allergy
Type 4, often known as late-type, allergies cause symptoms up to 72 hours after exposure. Allergic reactions often manifest as a red, itchy rash after skin contact with the offending allergen. The chemicals in things like costume jewelry, plastics, disinfectants, and cosmetics may enter the body and meld with the cells inside. Lymphokines, or special messenger chemicals, are released in huge numbers by sensitized T-lymphocytes when “contaminated” cells come into contact with them. These lymphokines then attract free cells, which kill the body cells along with the foreign substances. Areas of touch become inflamed, blistered, and itchy.
Who gets an allergy?
The mystery of the causes of allergies
Where does the fault lie? The natural world? That which runs in the family? Something like that? Allergists have worked tirelessly to uncover the root causes of allergies since their discovery. In 1916, epidemiological research provided the first hint that genetics could have a role. Almost half of those with allergies had relatives who also suffered from the condition.
Recent research supports similar findings, suggesting that there may be an “inherited” component to allergies. Asthma, hay fever, and neurodermatitis are hereditary, but the timing and severity of their onset are unclear; rather, it is the tendency to produce more immunoglobulin E in response to common allergens that runs in families.
The risk that a kid may acquire an allergy is higher if both parents are sensitive to grass pollen or another allergen. However, the child’s allergy does not necessarily have to be to the same allergen or cause the same symptoms. It has been shown through research involving over 7,000 sets of identical twins that siblings seldom have the same allergic reactions. However, only 5% of twins who share a parent have the same susceptibility to allergies.
In newborns, an elevated immunoglobulin E (IgE) blood level may be evaluated as an indicator of an allergy propensity; if both or either parent has allergies, the child’s risk of developing allergies is raised to 80%.
An estimated calculation of the likelihood of passing on an allergy susceptibility:
- Neither parent is allergic: 10 – 20 percent.
- One parent allergic: 30 – 50 percent
- Both parents are allergic: 40 – 75 percent
Whether or not this discovery constitutes an inevitable “destiny” is up for debate. Indeed, not everyone with increased IgE levels becomes sick. But what exactly decides who becomes allergic and why? Some allergy experts feel that the start of an allergy might be postponed, while others believe that the “power of genes” is so great that the environment plays only a minor role.
Genes or environment?
What about both?
Although the relative importance of hereditary and environmental variables in the development of allergies is still up for debate, most scientists believe that exposure to allergens in the environment has a significant influence.
In a baby’s first few months of life, it seems like its immune system is making a final decision on which things it will respond to. Foreign chemicals, such as allergens, may more readily penetrate the body’s defenses at this age since the immune system has not yet completely matured. Once they enter the circulatory system, they prime the immune system for an allergic response.
Young children who are genetically inclined to develop asthma may have even higher IgE levels if they are exposed to high levels of environmental allergens. House dust includes the extremely allergic feces of mites, and exposure to tobacco smoke, which damages mucosal membranes and makes them more permeable, seems to be especially stressful for these youngsters.
However, eating specific foods may greatly enhance that danger. According to research conducted in Finland, babies who are nursed for the first six months have a far lower risk of developing food allergies compared to their counterparts who are introduced to cow’s milk at a young age. Recent research has demonstrated that simply a single exposure to dairy products made from cow’s milk may set off an allergic reaction in youngsters who are already at risk.
Despite some major advancements in the field in recent decades, allergology still has a lot of questions that need answers. Why might recalling an allergy frequently be sufficient to cause symptoms such as hives or difficulty breathing? Is it possible that migraines might be caused by allergies as well? Can you explain the relationship between psychology and allergies and why it exists?
What makes a substance an allergen?
The relationship between proteins, pollen, and solubility in water
Almost everyone agrees that pollen, dust mites, and cat hair are perfectly safe and non-toxic. Why are they the cause of asthmatics’ wheezing attacks and hay fever sufferers’ itchy, watery eyes? Why do they cause allergic reactions? With all the advancements in contemporary allergology, this is still one of the issues that has no conclusive explanation.
While allergens may be found in pollen grains and home dust mites, it is well-established that it is not the allergens themselves that cause an allergic response. They are often proteins. Due to the fact that amino acids form very big molecules, they may easily penetrate the body through wet areas like the skin and mucous membranes.
Larger proteins seem to be much more allergenic than smaller proteins. It is not yet known why this is the case or whether an allergenic protein requires the presence of a certain amino acid or set of amino acids.
Proteins aren’t the only things that may set off an allergic reaction; non-proteins can do so as well, but only if they bind to proteins already in the body.
Allergenic proteins in pollen account for a negligible portion of the grain’s mass. The chemical components that make up a pollen grain are mostly insoluble in water and cannot enter the body. Although 15–20% of the proteins in a pollen grain or mold spore might trigger an allergic response, only a small percentage of those proteins are really responsible for the onset of symptoms.
Less than one percent of a pollen grain is composed of these so-called significant allergens. Secondary allergens are any residual potential allergies. Although they only have an impact on a small percentage of patients, they may be to blame for cross-reactions.
Humans have always had to deal with allergies like animal dander, dust mites, molds, and flower pollen since they are naturally occurring and not some recent “success” of the industrial era. But allergies to things like makeup, laundry detergent, or latex are obviously man-made. The prevalence of these chemicals means that allergy rates are rising with their usage. Studies in Switzerland and elsewhere have revealed that the percentage of allergy patients who respond to natural allergens has also grown dramatically. This does not explain the overall increase in allergies.
Analyzing an allergic reaction from an immunological standpoint
Of parasites, antibodies and exploding cells
Acute allergy symptoms include watery eyes, swollen nasal passages, or itchy skin. But what causes these reactions, and why can allergens that are safe for most people have such severe effects on those who are allergic to them?
The immune system proteins called type E immunoglobulins are to blame. They are part of our body’s vast “army” of antibodies, chemicals designed to ward against invading pathogens. Immunoglobulin E may account for less than 1% of total antibodies in a healthy individual, yet it plays a critical role in the body’s defensive mechanisms. Recent research suggests that they have a protective role against worm parasites.
Despite its many benefits, this “worm protection device” is not a gift for those who suffer from allergies. IgE antibodies were shown to be responsible for the bulk of acute allergy responses by researchers Kimishige and Teruko Ishizaka in 1966. Without an acute allergic reaction, the amount of these immunoglobulins E is up to 10 times greater in allergy sufferers compared to people who do not have allergies. The production of IgE almost explodes in response to interaction with an allergen.
Allergens enter the body via the respiratory system after being inhaled, such as pollen or house dust mite feces that has been agitated. There are several IgE molecules atop the surface of the local mast cells. Such a cell may be surrounded by 100,000–500,000 antibodies at once. These receptors detect allergens, and when they do, certain antibodies latch on.
To set off the mast cell’s planned “explosion,” all it takes is one allergen molecule to cross the narrow chasm between two antibodies at the moment of docking. When a cell bursts, it releases a surge of biological messenger molecules into the tissue, and the effects may be dramatic and rapid in certain cases. Histamine is one of the so-called mediators that causes an episode of hay fever by widening blood vessels and swelling mucous membranes. Other substances trigger contractions of the bronchial smooth muscles. Asthma symptoms include tightening of the bronchi and a subsequent decrease in airflow.
Some mediators and their effects
- Histamine: causes blood vessel dilation, an increase in vascular permeability, and bronchial constriction.
- Heparin: inhibits blood coagulation and the complement system is slowed by heparin.
- Prostaglandins: increased mucus production, vascular permeability, permeability, and inflammation are all effects of it.
- Leukotrienes: causes an increase in mucus production and a spasm of smooth muscle.
- Platelet activating factor (PAF): causes granulocyte adhesion and narrowing of vessels.
An accurate understanding of these pathways underpins several treatments for the signs of an allergic reaction. They work by inhibiting the receptors for certain mediators or by striking at the mast cells themselves.
The immune system’s protective cells
Regarding killers, macrophages, and the key-and-lock hypothesis
When it comes to warding off pathogens from the outside world, the human body deploys a whole army of defense cells. They coordinate the body’s defensive strategy by exchanging messages via the lymphatic system.
Macrophages
Macrophages are the first line of defense against foreign bodies that enter the body. These immune system “eating cells” circulate as monocytes in the circulation and are found in almost all human tissues. Whenever they encounter a foreign antigen, such as a microbe, they will engulf it and digest it. They also secrete a variety of powerful chemicals that draw in other crucial repairing and defending cells.
In addition to serving as the body’s general “health police” and “clean-up command,” neutrophils play a critical role in the start of an antibody response by bringing antigens from the digestive tract to the lymph nodes.
Lymphocytes
Lymphocytes, a kind of “white blood cell,” are the major “agents” of the immune system’s specialized defenses. The lymphoid cells that make up just 2% of an adult human’s total body weight number slightly over a thousand in type. Lymphocytes begin their lives in the bone marrow like all other blood cells, but they must undergo further development and differentiation to become fully functional immune defense cells.
Some of these progenitor cells move from the hematopoietic organs to the thymus gland, where they mature into the so-called T lymphocytes. There, they get the ability to identify both healthy and harmful cells in the body. The remaining lymphocytes develop into “bone marrow-derived” B cells while staying in the bone marrow.
Lymphocytes’ capacity to respond to a specific kind of molecule using the key-lock principle is perhaps their most valuable characteristic. They’re outfitted with sensors on their surface (the “lock”) that are tailored to the shape of any one of a zillion possible invaders (the “key”). The production of new “locks” is the job of T cells. When presented with a “new invader,” macrophages use the intricate structure of cellular and foreign proteins on their surfaces to identify the antigen as “new and foreign,” and they then activate the appropriate immune response.
As a response to this “new” foreign substance, the body produces T-killer cells that seek out and destroy it. The body’s “antibody factories,” or plasma cells, are produced by B lymphocytes, which are stimulated to do so by T-helper cells. Even though their lifespan is just a few days, during that period they may release hundreds of specific defensive chemicals each second.
Some of the B cells “remember” the foreign material and may begin generating the right antibodies immediately the next time the immune system comes into contact with it. Most preventative immunizations rely on this same “secondary immune response.”
Humoral immune defense and antibodies
Protection from the guardian molecules
Antibodies are one of the immune system’s “primary weapons,” alongside phagocytes and killer cells. The big Y-shaped protein molecules circulate freely in the bloodstream and may dock onto the surface structures of the invasive foreign substances using the lock-and-key concept. In either case, the “occupied” chemicals are rendered useless or marked so that macrophages and killer cells may more readily identify and eliminate them.
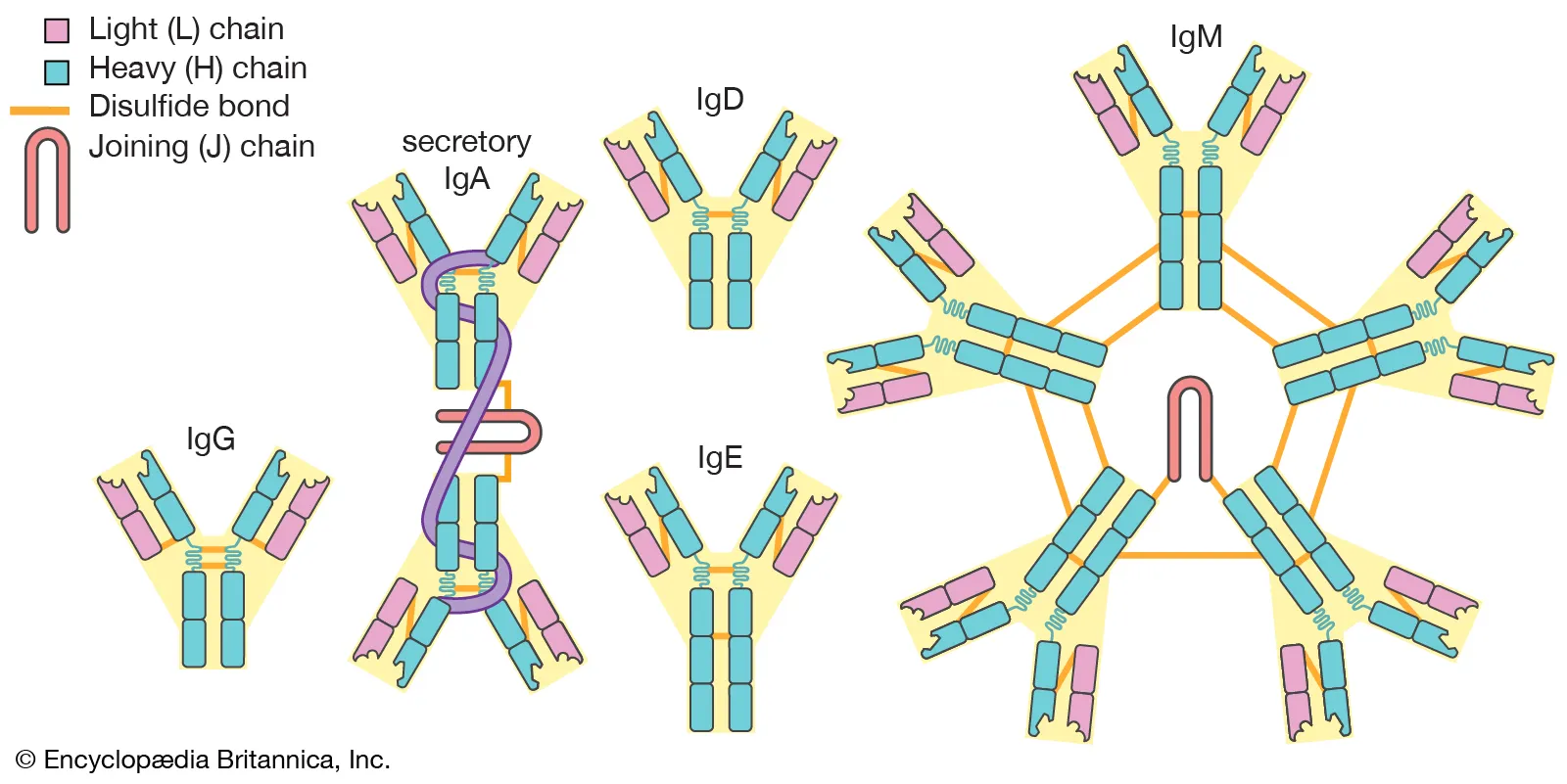
The immune system of someone with allergies is overreacting because specific antibodies can no longer tell the difference between safe and hazardous invaders. There are millions of distinct antibodies in the human body, but only one will work against any given antigen. Whether an “intruder” is already recognized by the immune defense system or whether it is a “new opponent” determines if the necessary defense molecules are already present in the blood or whether they must be freshly created. Besides their targeted antigen specificity, five broader kinds of antibodies may be identified.
Immunoglobulin G antibodies are the most prevalent and crucial ones found in the blood (IgG). In conjunction with immunoglobulin M, they encase bacteria in a protective sleeve, making them harmless even if they find their way into the tiniest cracks of a host’s tissue. To do this, both immunoglobulins combine with bacterial surface antigens to produce a complex that triggers the release of a specific enzyme in the blood. This sets off a cascade of responses termed complement reactions that destroy the bacterial cell by destroying its membrane.
The class of antibodies responsible for the acute allergic response is known as type E immunoglobulins. Their “heavy” chains are designed in such a manner that they may cling to the surface of the so-called mast cells very well.
Histamine, a tissue hormone that, for example, causes the arteries to widen in cases of inflammation, is present in and produced by these cells, which are prevalent in the blood and mucous membranes. Consequently, defense cells will have easier access. Among other things, the release of histamines stimulated by IgEs is what causes the mucous membranes to expand during acute allergy reactions.
Saliva and tear fluid are largely where you may get immunoglobulin A. By preventing pathogens from accessing the mucous membranes, it ostensibly defends the respiratory system and digestive organs.
Immunoglobulin D‘s function is still mostly unclear. However, as these antibodies are mostly included in cell membranes, they could be crucial in controlling membrane activity.
Bibliography
- Maleki, Soheilia J; Burks, A. Wesley; Helm, Ricki M. (2006). Food Allergy. ISBN 978-1-55581-375-8.
- Pongdee, Thanai. “Increasing Rates of Allergies and Asthma”. American Academy of Allergy, Asthma & Immunology.
- “Allergic Diseases”. NIAID. 2015.
- Grammatikos AP (2008). “The genetic and environmental basis of atopic diseases”. Annals of Medicine. doi:10.1080/07853890802082096.
- “World Allergy Organization”. Archived.
- Sinn, John KH; Osborn, David A. (2007). Osborn, David (ed.). “Prebiotics in infants for prevention of allergy and food hypersensitivity”. doi:10.1002/14651858.CD006474.








