There is a reason for optimism for those with dementia. A novel monoclonal antibody has shown positive results in treating Alzheimer’s disease in its earliest stages. Lecanemab was shown to decrease cognitive decline by roughly 27 percent in the phase 3 clinical study, and it also reduced dangerous amyloid plaques in individuals with dementia. There was also a significant decrease in the occurrence of serious adverse events such as brain hemorrhage and edema compared to two other antibody formulations examined for Alzheimer’s disease.
The gradual death of brain cells, or Alzheimer’s dementia brought on by misfolded amyloid and tau proteins is still incurable and cannot even be halted. Despite the fact that numerous active compounds have shown promise in animal experiments, they have often underwhelmed in testing with humans. Both of these treatments either did not effectively slow the progression of dementia or had unacceptable adverse effects.
Anti-dementia antibodies

This has been the case with the most recent therapeutic tool in the arsenal against dementia as well. Antibodies. These immune proteins were engineered in a lab to specifically bind with and eliminate the misfolded proteins that are characteristic of Alzheimer’s disease. The amyloid plaques of Alzheimer’s disease patients have responded well to antibody preparations including aducanumab, donanemab, and gantenerumab in early clinical studies.
The difficulty is that although these antibodies were successful in reducing amyloid plaques in clinical studies, they typically failed to decrease dementia as well. Additionally, all antibody preparations have major and occasionally fatal adverse effects, including cerebral edema and microhemorrhages. The European Medicines Agency (EMA) has rejected the antibody preparation aducanumab on the grounds that the hazards outweighed the benefits.
Lecanemab antibody study
However, recent success in a phase 3 clinical study of an antibody created by a team headed by Christopher van Dyck of the Yale School of Medicine offers renewed optimism. Lecanemab is a combination of monoclonal antibodies that are highly selective for amyloid beta protofibrils. There is evidence to suggest that these misfolded proteins, which appear as filaments, play a role in the development of amyloid plaques.
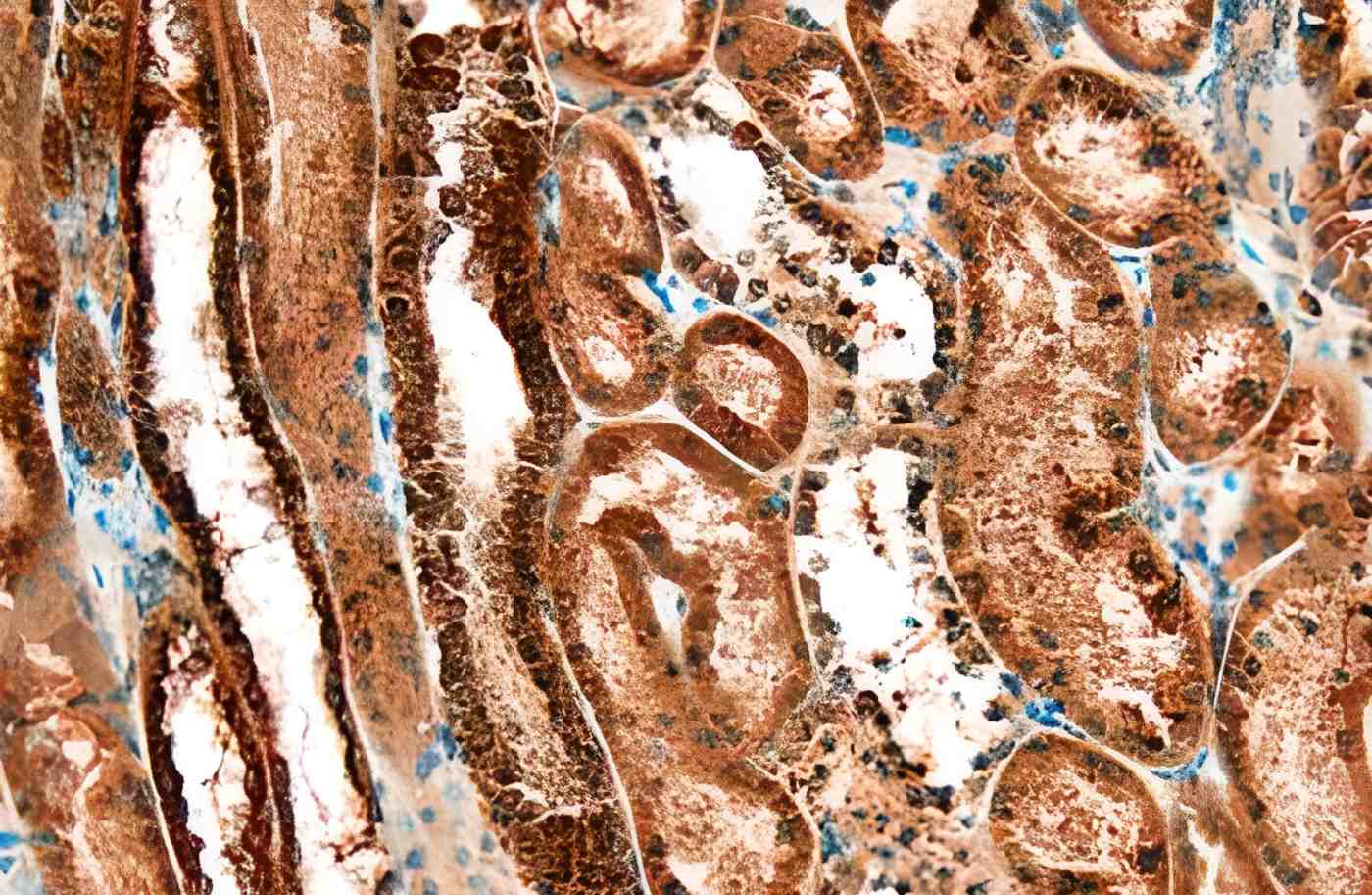
A total of 1,785 individuals with moderate Alzheimer’s dementia were given lecanemab antibodies through biweekly infusions or a placebo. Researchers used positron emission tomography to regularly scan participants’ brains over the course of 18 months, measuring amyloid deposit density and volume (PET). In addition, at the start of the trial and at regular intervals thereafter, all patients were given a battery of standardized tests measuring different aspects of their cognitive functioning.
Decreased dementia and plaque formation
After 18 months of therapy, those who received the antibody had much less amyloid plaque growth in the brain than those in the control group. In addition, their mental deterioration slowed by 0.45 points on the so-called CDR-SB scale of 18 points. According to the researchers, this translates to a 27% reduction in dementia and a 37% reduction in ADL impairment (Activities of Daily Living).
The current trial demonstrates the most convincing evidence of effectiveness for lecanemab among the three antibodies (aducanumab, gantenerumab, and lecanemab). But it’s true that initially, the patient is unlikely to feel this influence particularly strongly in their day-to-day existence.
However, there is a bigger picture: If the impact continues, the gap will widen over time, making the initial discrepancy much more significant. Throughout the course of the 18-month trial, it became clear that the discrepancies between the treatment and placebo groups grew.
Antibodies with fewer negative effects
However, adverse effects may be a deciding factor in the approval process. Exaggerated immunological responses occurred with lecanemab soon after infusion, similar to earlier antibody preparations, although they were often neither severe nor enduring. On the other hand, lecanemab has also been linked to brain swelling and bleeding. Researchers found that 21.3% of the time they occurred. However, the vast majority of them were symptom-free and could only be identified by a brain scan.
Consequently, it seems that lecanemab results in less cerebral edema and microbleeds than other antibody preparations. When compared to other antibodies, lecanemab has a lower incidence of such ARIA. The researchers found that the benefit-risk ratio of lecanemab improved due to the drug’s relatively low risk.
But will lecanemab be approved as a treatment for Alzheimer’s disease? The last stage before an application is often a “phase 3” trial. However, van Dyck and his group remain cautious and suggest doing more, longer-term research first. The researchers need to wait for clearance before they can submit an application for this study.
On the other hand, Schulz is certain that lecanemab will join the approval procedure in the near future since the statistics are so compelling and consistent, and the recorded adverse effects are quite minimal.
The turning of the tide for antibody treatments to treat Alzheimer’s
Despite these limitations, the new antibody formulation represents a promising advance in this relatively novel approach to treating Alzheimer’s disease. These findings represent a watershed moment for the reason that they prove that modern antibody treatments are making progress toward their objective of eliminating amyloid plaques and halting the progression of dementia.
The authors and commentators on the paper agree that lecanemab’s targeting of amyloid protofibrils, rather than amyloid plaques, is a significant step forward. It is believed that the progression of dementia in the brain is related to the presence of these misfolded beta-amyloid filaments, which are especially harmful to cells.
It’s believed that Alzheimer’s disease begins with the first stages of Alzheimer’s plaques damaging nerve cells. On the other hand, the plaques should be left alone since they are evidence of successful elimination of the harmful early stages.
(NEJM 2022; 10.1056/NEJMoa2212948).