Who doesn’t anticipate nice summer nights and wearing a T-shirt outside? Rising temperatures and longer days also signal the return of some less welcome neighbors: bloodsucking insects like mosquitoes, ticks, flies and others that hibernate throughout the winter. Yet the mini vampire bites aren’t only irritating; they may also spread deadly infections. Scientists are still scratching their heads over how the creatures know to repeatedly choose a good host, and it is unclear which elements contribute to this. Several repellents have been developed over the years to ward off these bloodsuckers.
- Vampires of the animal kind
- Searching for food among the obstacles
- Chemical signals for locating the hosts
- Where do the differences in “attraction” come from?
- Drilling methods used by the insects
- Diseases spread by tick and fly bites are on the rise
- The Lyme disease
- Tick-borne encephalitis (TBE) disease
- The Malaria disease
- Other diseases spread by bloodsuckers
Vampires of the animal kind
It’s a warm summer night, and you and your pals are relaxing on the patio or in the beer garden. Sadly, just as things start to seem comfortable, the unwelcome guests — mosquitoes — show up. They swarm about us, making piercing noises, and repeatedly attempt to land on our exposed flesh from a low altitude.
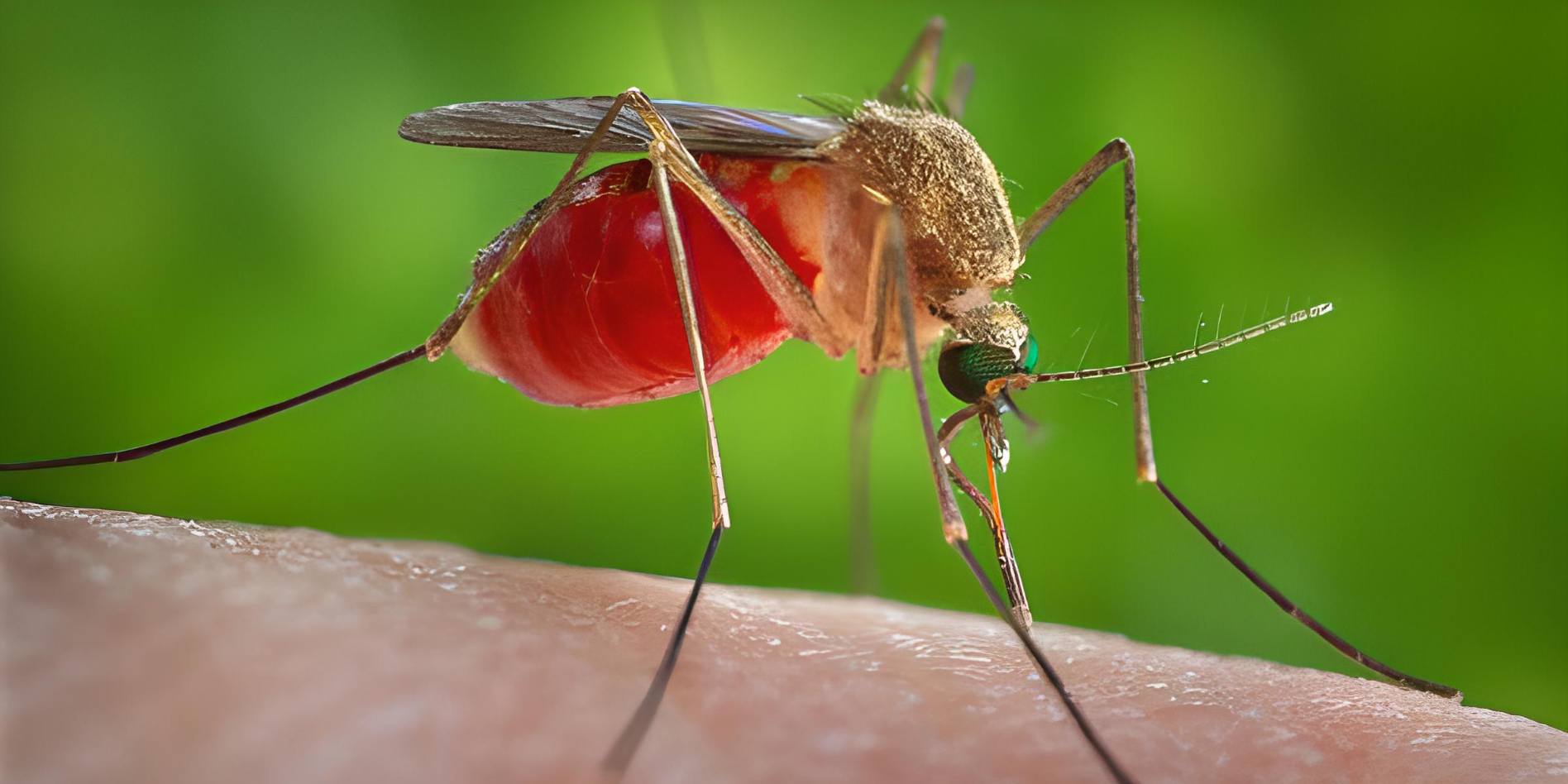
Even if you wave and yell, the flying little bloodsuckers just need a second of your attention to bite. The end effect is red, itchy wheals that will keep you busy for days. Such bites are more bothersome than hazardous in many countries, but in other parts of the globe, they may spread malaria and other deadly infections.
However, humans are not safe from the bloodsucking insects’ assaults at any time of day or night; certain mosquito species, such as Aedes aegypti, which is endemic to warmer climates, are diurnal and bite more often in the morning and late afternoon. Midday horseflies are just as relentless in their pursuit of “victims” as their nighttime counterparts, and may deliver a painful bite. When they bite, mosquitoes are so small that you can hardly sense them.
Some bloodsuckers, however, are more stealthy in their methods: ticks “lurk” for passing victims in the dense grass and bushes of woodland clearings or embankments, as well as in your own garden. They don’t just fall out of the trees as myth has it, but rather hide out in the path of oncoming vehicles to be wiped down. Their bites aren’t painful most of the time, but they may have devastating effects if the tick was infected with a virus or bacterium during its blood meal. Tick-borne illnesses, including meningitis (TBE, tick-borne encephalitis) and Lyme disease, are prevalent in many countries.
Because of this, researchers at universities, tropical research centers, and pharmaceutical businesses are continuously on the lookout for new and improved methods of protecting humans and animals against bites from mosquitoes, flies, ticks, and other bloodsucking pests. For these to be created, however, scientists require a better understanding of how the “bloodsuckers” locate their prey, the “signposts” they employ, and why they find certain humans more alluring than others.
Searching for food among the obstacles

To obtain its blood meal, a bloodsucker must first overcome a number of obstacles, such as finding a host that carries the right food cocktail, finding the best place to puncture the host, overcoming the host’s immune system’s defenses, escaping the host alive, and digesting the large amount of blood it has consumed. A bloodsucker animal’s existence is fraught with difficulties.
To a tick or other bloodsucking bug, a person is only a delivery system for the nutrient-rich blood within. However, since this blood is not detectable at greater distances, the animals must rely on other “tracks” to identify their hosts. Some species employ optical signals, others chemical ones, yet others thermal ones, and still others a mix of these.
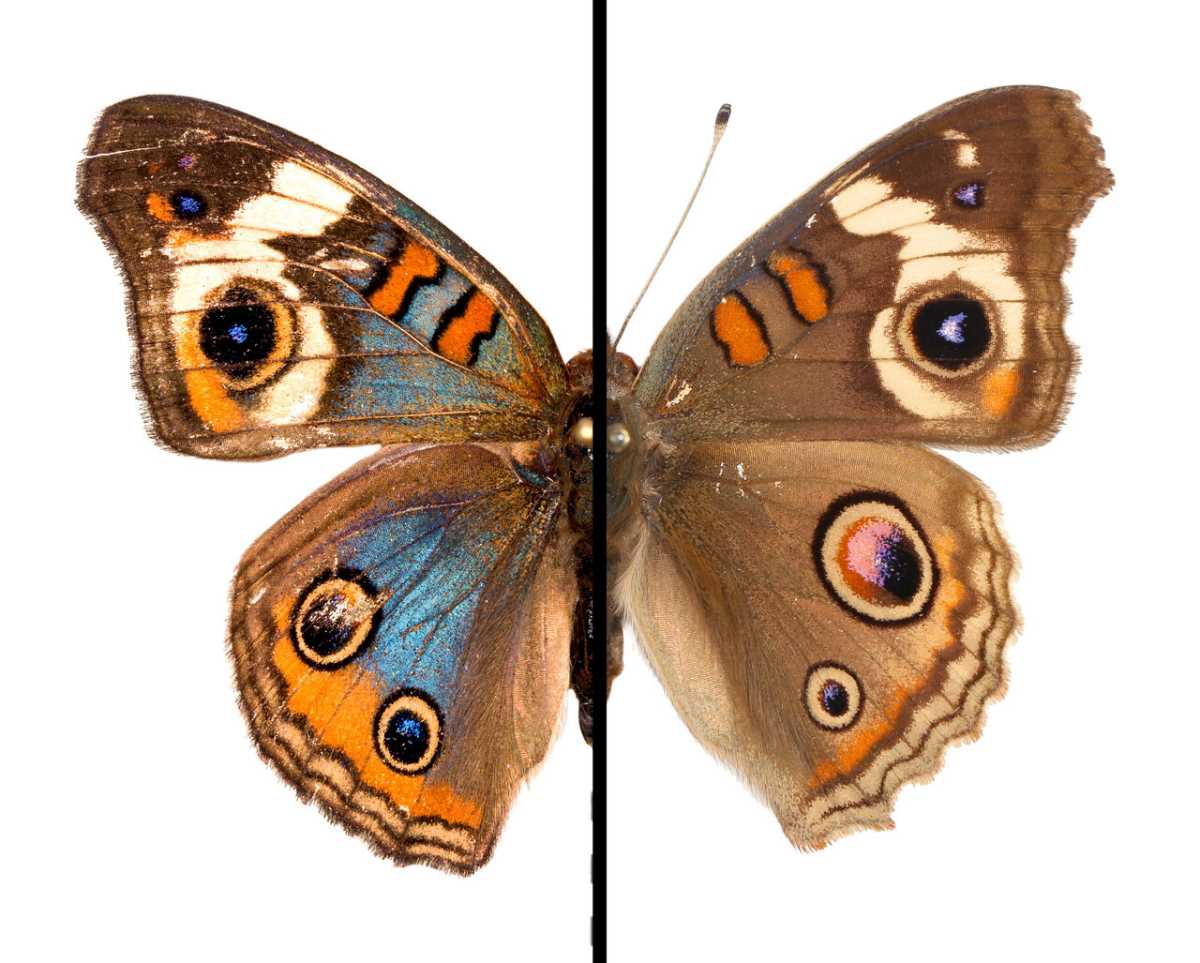
Many day-biting insects use color and shape as a primary cue to locate their prey; horseflies, which hunt mostly in open terrain, are attracted to huge bodies that rise above the horizon and may use this information to locate grazing cattle or horses, which provide an ideal source of blood.
Tsetse flies, found only in the tropics, utilize very similar signals to communicate with one another. Some scientists believe that since zebras are so vulnerable to biting insects, their distinctive striped pattern evolved as a defense strategy. This is because the zebra stripes confuse the predator’s visual perception of the body, making it harder for the insects to zero in on their intended meal.
The visibility of optical signals drops dramatically at night. As a result, many nocturnal bloodsuckers rely on the radiant heat given off by warm-blooded animals or people as a source of navigation. Mosquitoes, while looking for a human host inside, will often fly in tight circles toward the ceiling. When they detect a current of warm air, they will often dive into it to get closer to their intended prey.
Chemical signals for locating the hosts
A very special scent
However, the scent is a vital stimulant for almost all bloodsuckers. Their primary environmental triggers are waste materials generated by living organisms. Insects are particularly drawn to the carbon dioxide exhaled during exercise, but they are also drawn to other compounds exuded during physical exertion, such as water vapor and substances in human perspiration, such as lactic acid or its bacterial breakdown products.
Since people and animals do not consistently release these odors, pinpointing their location using them is difficult. Instead, the activity level influences the production of erratic fragrance streams that are carried by the wind. Since mosquitoes can’t sense uniform gradients, they have to navigate by repeatedly visiting different “scent islands” in search of food.
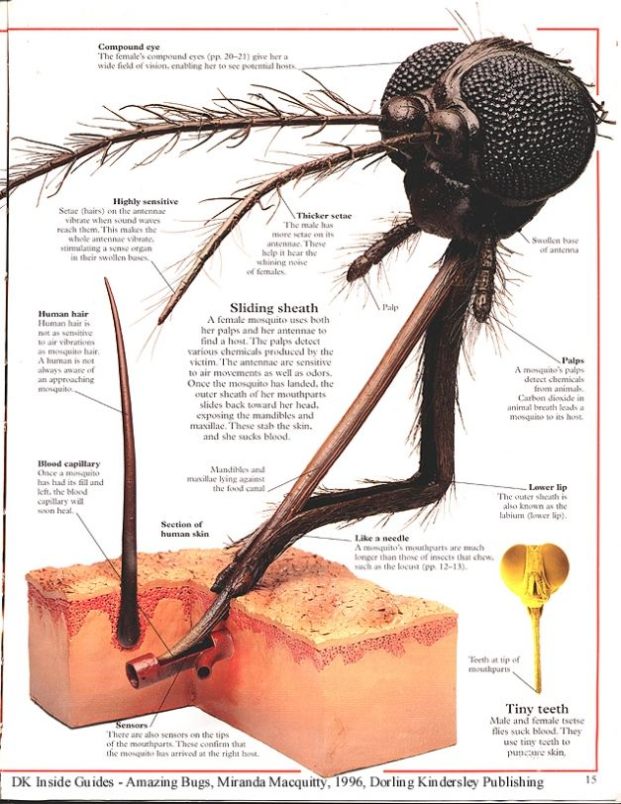
A mosquito’s chemoreceptors are so sensitive that they can sense minute fluctuations in the air’s carbon dioxide level. It has been shown that even a 0.01 percent rise in CO2 may elicit a response from the animals in wind tunnel trials, where they would then engage in their normal seeking activity. They fly directly in the direction of the increasing gradient so long as they are inside a “scent island,” but when they enter a zone of decreasing concentrations, they suddenly shift flight direction and keep doing so until they reach a zone of increasing concentrations again. Mosquitoes can still detect and respond to olfactory cues at distances of 65–115 feet (20–35 m), while tsetse flies can do so at more than 300 feet (90 m).
While chemical sensing, particularly of carbon dioxide, is a widely used and vital host-finding strategy for insects and ticks, most bloodsuckers use more than one signal at once. To pinpoint their prey, mosquitoes use a variety of sophisticated navigational tools. According to mosquito experts, they discern between brightness, form, color, temperature, humidity, carbon dioxide content, and the concentration of odorants in the air released by the objects of their desire.
Where do the differences in “attraction” come from?
Sweet blood
Why are some individuals actually “mosquito repellents,” who get bit constantly, while others are seldom bitten if at all? Not even scientists can agree on the precise mechanism through which this effect operates. One thing that can be said with absolute certainty is that “sweet” blood has zero bearing on this.
In lab experiments, there was no correlation found between blood type or blood sugar levels and the mosquitoes’ inclination to bite. Instead, it appears that each person’s unique combination of amino acids, amines, steroid hormones, and other metabolic products provides an enticing aroma to mosquitoes and other biting insects.
However, mosquitoes may pick up on even subtle changes in body temperature as a signal. In the experiment, a change in temperature of only a tenth of a degree was enough to change the mosquitoes’ biting habits. The fact that males attract mosquitoes in the lab more than women may be explained by this finding. This is because, particularly at night, men tend to have a somewhat higher core temperature than women. However, males are less likely to be bitten than women since their body hair is thicker.
It has been shown in the lab that mosquitoes are more likely to bite a woman between the 13th and the 18th day of her menstrual cycle, coinciding with the time when the female reproductive system is most active. But whether this is because of a rise in estrogen levels in the blood or a concomitant rise in body temperature is still unclear.
Drilling methods used by the insects
An axe or a straw
The mosquito or tick has not yet arrived at its target just because it has located its host and settled on it. It has to find a good spot to penetrate the host’s skin and make sure the host is a good fit before it can bite.
Ticks will spend hours searching “their” people for areas of thin skin to feed on. After landing on your ankles or lower legs after being stripped in thick grass or shrubs, they will climb up your body and bite you where it hurts the most: in the inner thighs, armpits, or neck. The small arachnids have a very low chance of being discovered since they migrate when concealed by clothes and their crawling is scarcely perceptible.
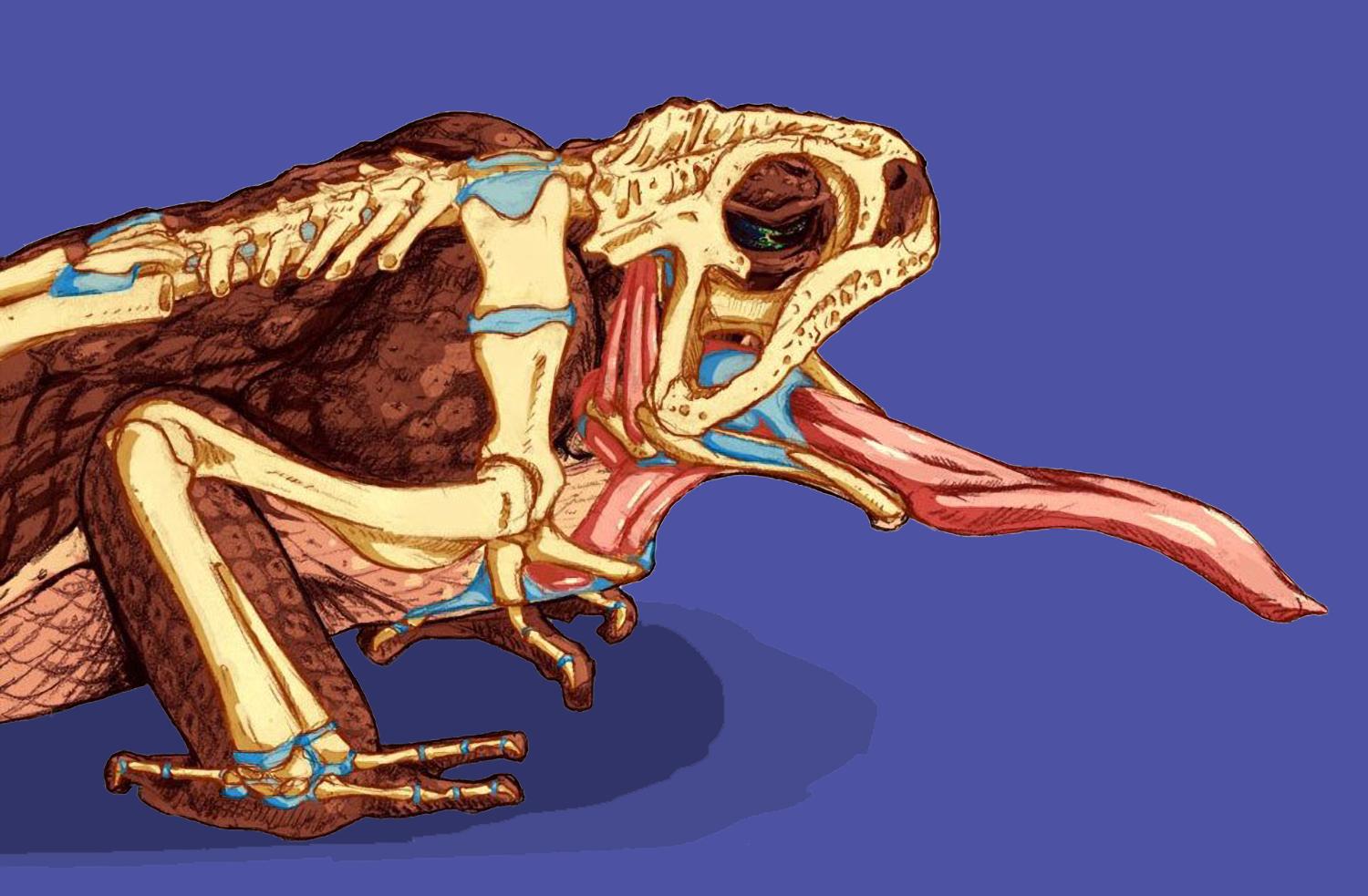
However, mosquitoes, horseflies, and most other flying bloodsuckers are distinct in that they tend to stay around where they land and bite. Since they are quickly detected and chased away or killed unless their target is sleeping, speed might be (super-) vital for them. Still, before beginning to really feed, mosquitoes conduct a series of “test bores” to assess the surrounding environment. The closest blood capillaries beneath the skin may be detected by the insects thanks to taste receptors located at the end of their proboscis.
Bloodsuckers use two methods to get at the blood that is protected by numerous layers of skin and tissue. The “axe” method is used by ticks, horseflies, and others like them; these insects utilize their modified mouthparts, which resemble scissors, to rip the layers of skin that protect the tiny blood arteries under the skin. The victim of one of these not-exactly-gentle bites will naturally fight back since pain is definitely being felt.
However, the bloodsuckers have evolved to deal with this: horseflies and ticks are resistant to not just gentle hand strikes or a whack from the cow’s tail, but also being rolled over. Ticks, on the other hand, must take extra precautions to avoid being discovered and removed since they feed for many days rather than seconds. Since their saliva includes an anesthetic and chemicals that inhibit the victim’s immunological reaction, the unmistakable itch is not present. Simultaneously, they secrete a white, fast-hardening substance into the wound that “cements” their mouthparts into the skin of the host, keeping them from being torn off.
Supporters of the “straw approach” are much more astute: The proboscis of a mosquito or tsetse fly is surrounded by sharp parts, allowing them to incise the skin of their prey and target specific blood vessels. Sucking injects saliva into the sting site, which prevents blood clotting and enhances the permeability of the capillary walls, assuring a plentiful flow of blood.
Mosquito bites itch because your body is reacting to the foreign proteins in the mosquito saliva. This usually happens three minutes after being bitten. As a rule, the victim of a mosquito bite doesn’t realize he’s been bitten until after the mosquito has already completed draining all the blood out of his body (which takes just two to three minutes).
Diseases spread by tick and fly bites are on the rise

As soon as a mosquito or tick has had a successful blood meal, the situation is typically over for it. However, people don’t fare so well, and they may be left with far more dangerous mementos than just itchy pustules if they’re not careful. This is due to the wide variety of harmful infections that may be transmitted by the biting of insects like mosquitoes and ticks. Malaria, yellow fever, leishmaniasis, and dengue are just a few of the illnesses that these mosquito-like pests are responsible for spreading.
However, in many countries, ticks are the primary vectors of illness due to their ability to transmit both the meningitis-causing TBE virus and the Lyme disease-causing Borrelia burgdorferi bacterium via their saliva. It is believed that between 1% and 20% of the population in developed countries is infected with TBE, whereas 30% of ticks in many developed countries contain Lyme disease viruses.
However, most mosquito-borne illnesses or their related vector species are not endemic to a specific region, so most people do not need to worry about serious long-term implications from a mosquito bite. But ongoing climate change may cause that to change. Epidemiologists are concerned about a rapid expansion of present endemic regions due to the fact that climate substantially influences the transmission of both the viruses and their animal vectors.
Malaria deaths increased by 12% to an estimated 627,000 in 2020, compared to 2019 figures. For illnesses transmitted by ticks, such as dengue fever, similar patterns have been seen. The fact that malaria cases also often rise in regions where higher temperatures and more precipitation are recorded during the El Nino phenomenon.
For the first time, a 36-year study on tick-borne meningitis has shown what experts consider to be a direct connection between climatic data and the spread of TBE. The majority of the reason why more and more infected ticks are surviving, according to experts, is that winters in temperate and northern latitudes are becoming milder.
A mosquito or tick bite might have much more devastating effects in the future than it does now if this trend is proven for other illnesses as well. According to epidemiologists at Harvard University’s model estimates, the temperate zones of Europe, North America, and Asia are expected to see the most shifts. The risk of malaria infection might quadruple in the tropics and potentially increase more than tenfold in temperate places if the global temperature climbs by three to five degrees by 2100, as projected by the IPCC climate scientists.
The Lyme disease
The most prevalent tick-borne illness is Lyme disease, which is brought on by the bacterial pathogen Borrelia, which is present in five to 35 percent of European ticks. Although Lyme disease symptoms have been reported since the early 20th century, Willi Burgdorfer did not identify the illness’s underlying cause until 1981.
Pathogen:
The bacteria Borrelia burgdorferi, which is a member of the Spirospecies group, is what causes Lyme disease. The slow-growing, corkscrew-shaped bacteria are distantly related to the syphilis pathogen. There are now at least ten distinct species of Borrelia, among which B. afzelii, B. burgdorferi sensu stricto, and B. garinii are thought to be the major culprits behind Lyme disease.
Distribution:
Lyme disease occurs in all temperate zones of the world. The USA, Canada, and a sizable portion of Eurasia are regarded as endemic regions in the northern hemisphere. Other countries in Central Europe also face a high risk of infection.
Transmission:
The primary vector of Borrelia is the tick Ixodes ricinus, sometimes known as the wood tick or sheep tick. When ticks feed on an infected bird, rodent, or other small animal as a larva or nymph, they acquire the infection. These are known as “reservoir hosts,” and since they can carry Borrelia without developing Lyme disease themselves, they are crucial intermediary hosts for the infection.
When an animal pumps extra fluid it has taken along with blood back into the wound, the Borrelia also travels there from its digestive system and is often not transferred to people for 24 to 48 hours after the tick bite.
Although there is a higher chance of infection in the spring and autumn, tick activity may theoretically continue throughout the year if there is a warm winter and a chilly, humid summer. Tick season may start as early as late March or as late as April, depending on the weather, and it lasts until the animals start to hibernate in the late autumn.
Symptoms:
Stage 1:
An erythema migrans or wandering redness of the skin that appears days to weeks after a tick bite is a common early indication of a Borrelia infection. The redness, which is present in around 60% of cases, steadily develops around the bite site and, in severe instances, may have a circumference of up to 30 inches (75 cm). Flu-like symptoms, including fever, headache, limb discomfort, and lymph node enlargement, may also manifest at the same time. Even without therapy, these symptoms go away after a while.
Stage 2:
After initial infection, the virus may take anywhere from a few weeks to a few months to travel throughout the body through blood and lymph, eventually affecting the nervous system, muscles, and joints. Along with a general sense of sickness or weakness, this may result in inflammation of the heart muscle, meningitis, encephalitis, or even paralysis of the limbs or face.
Stage 3:
Chronic Lyme disease may appear months or years after the first infection. Invasive infections are to blame, since they establish themselves in inaccessible parts of the body. Lyme arthritis and acrodermatitis atrophicans (skin thinning and discoloration) are the most prevalent long-term consequences of contracting Lyme disease. Heart muscle injury and persistent meningitis are also conceivable, albeit uncommon.
Treatment:
Antibiotics are most effective in the early stages of an illness, when the condition is still relatively simple. Depending on the intensity of symptoms, therapy might last anywhere from two to four weeks. It is much more difficult to treat Lyme disease after it has progressed to the chronic stage because, by that point, the germs have moved to less easily accessible tissues in the body. However, health organizations caution against the practice of taking antibiotics after every tick bite.
Prevention:
As of yet, there is no preventative vaccine available for Lyme disease. A vaccination (LYMERix) protecting against the bacterium’s outer membrane protein was developed in the United States but was discontinued by the manufacturer in 2002.
Avoiding being bit by a tick in the first place is the best way to stay healthy. Scanning one’s whole body after returning from time spent in the outdoors may, however, significantly lower one’s chances of contracting an infection.
Tick-borne encephalitis (TBE) disease
Meningoencephalitis (Meningitis) caused by ticks is the most serious tick-borne illness throughout the spring and summer months.
Pathogen:
TBE, or summertime meningitis, is caused by a flavivirus. The roughly 70 viruses in this genus are responsible for a wide variety of human illnesses. These viruses are often spread by mosquitoes and ticks. The dengue and yellow fever viruses, as well as the hepatitis C virus that is not spread by insects, fall within this category as well.
Distribution:
Wide yet the isolated distribution is typical of TBE. So-called “natural herds” are pockets of the virus where the local reservoir has been stable for years. The Robert Koch Institute (RKI) reports that several regions of central Europe have an abnormally high rate of infection. Up to 10% of ticks in these regions carry pathogens. High-risk regions are defined by epidemiologists as those with 25 or more cases.
But the RKI’s yearly map of TBE risk zones may not accurately depict the pathogen’s true spread. There are research doesn’t rely on illness cases, but rather on the investigation of more than 10,000 ticks and the blood of almost 5,000 forest workers. Animals afflicted with TBE were discovered in areas previously assumed to be TBE-free, and the number of ticks infected with the disease was determined to be at least 10 times higher than previously thought.
Transmission:
TBE is transmitted mostly across Europe by Ixodes ricinus, also called the wood tick or sheep tick. Rarely, the virus may also be transmitted via the consumption of raw milk from infected cows or goats. One to five percent of ticks in most TBE regions carry the virus. Sucking on an infected bird, rodent, or other small mammals as a larva or nymph is how the animals get infected. These so-called reservoir hosts are crucial because they may transport TBE viruses without being infected with meningitis.
Transmission of the TBE virus occurs rapidly, usually within a few minutes after a bite. First, the tick’s anesthetic saliva tears open the skin, allowing the germs to be delivered into the wound. However, not everyone who is bitten by an infected tick will become sick. Only approximately 30% of affected people show symptoms.
Symptoms:
There are two stages to the disease’s development: Mild fever, headache, and vomiting like the flu develop after an incubation period of one to two weeks. However, within a short period of time, these symptoms diminish and, in most instances, the sickness is cured. But the virus may also cause meningitis in certain people by spreading to the brain and spinal cord. High temperatures, pounding headaches, and neck stiffness are all symptoms, but within a few days, most people recover completely.
However, in rare but severe instances, the virus causes inflammation of the brain (meningoencephalitis), which may be accompanied by cognitive difficulties, mood swings, or even the beginnings of paralysis. Ten percent to twenty percent of people with severe TBE have lasting cognitive impairment; one to two percent of people with TBE die from the condition.
Treatment:
TBE, like many viral illnesses, has no effective treatment options. Unfortunately, once an outbreak has occurred, medical treatment is limited to symptom relief.
Prevention:
The TBE vaccine is very effective. Therefore, institutions suggest that vacationers and locals alike get the TBE vaccine before visiting an at-risk location. Those who spend their days in the woods or countryside, or who engage in tick-risky hobbies like hiking, horseback riding, or cycling, are at the greatest risk of contracting Lyme disease. Until recently, the vaccine against TBE had too severe of an adverse effect to be administered to children younger than 14. However, new active chemicals have just been introduced to the market, and the Federal Office for Sera and Vaccines strongly encourages their use, at the very least for children in high-risk locations.
Vaccination may be administered even after a potentially infective tick bite has occurred, in addition to active immunization, which comprises three separate vaccines and gives protection for three years. Immunoglobulins, molecules of the immune system that are meant to make the virus harmless, are directly injected rather than attenuated pathogens. However, this passive immunization is only effective for up to 96 hours after the bite, and only in roughly 60% of instances. Preventing a tick bite in the first place by donning protective gear and making use of chemical repellents is therefore an essential aspect of proactive safety measures.
The Malaria disease
From 2000-2015, the annual mortality toll from malaria decreased by over 40% to 562,000 (from 896,000), as reported by the World Health Organization. It’s no exaggeration to say that malaria is among the most important infectious illnesses ever. The World Health Organization estimates that around 600,000 individuals a year lose their lives due to malaria today.
Pathogen:
Malaria is caused by a parasitic protozoan of the genus Plasmodium, not by bacteria or viruses. Malaria tropica, produced by Plasmodium falciparum, Malaria tertiana, caused by Plasmodium vivax, and Malaria quartana, caused by Plasmodium malariae, are the three most common kinds of malaria.
Plasmodia are intracellular parasites that damage human red blood cells as they grow. They complete the last stages of their development in Anopheles mosquitoes.
When a mosquito feeds on the blood of a person afflicted with malaria, it also consumes Plasmodium gametes. These develop and merge in the animal’s digestive system. The resultant cell is mobile and is able to invade the muscle tissue outside of the mosquito’s digestive system. Here is where the cell splits many times to produce the sporozoites that will act as the carriers. They enter the mosquito’s salivary gland and are then transferred to the victim’s skin when the insect bites again.
Sporozoites in humans go from sites of injury to cells in the liver, spleen, or bone marrow, where they mature before entering the bloodstream and invading red blood cells. They replicate within the blood cells and kill them in the process. There may be many cycles of this process before the Plasmodium gametes are also generated in blood cells, but it may happen. When the mosquito consumes them during its blood meal, the cycle is complete.
Distribution:
Malaria is widespread in the tropics and subtropics. Malaria affects more than 25 percent of the world’s population, who reside in one of more than 100 nations classified as endemic. More than 90 percent of the world’s malaria cases are reported in Africa. In contrast to Africa, where malaria rates have been almost stable, infection rates have risen in other parts of the globe.
Malaria was formerly widespread over all of Europe; throughout the Middle Ages, it ravaged England, and reports of it spreading to Sweden and Finland date to the 18th and 19th centuries. Malaria did not stop being a problem in northern and central Europe until the 20th century. The widespread use of DDT after World War II to clear marshes and reduce mosquito populations was a major factor. Eight hundred to a thousand cases of malaria are recorded in countries now. Malaria is spread primarily via the introduction of infected travelers from malarial regions.
Transmission:
Malaria parasites are spread by the bite of an infected female Anopheles mosquito. Although there are over 70 species of Anopheles that might be classified as vectors, the most significant and prevalent in Africa is Anopheles gambiae. Although several Anopheles species are common in the region, they are not currently thought to be carriers of disease. Occasionally, infected mosquitoes may be brought onto an airplane as “stowaways” in the baggage of passengers and live for a while until they are killed. Airport malaria is the outcome of a bite from one of these insects on a person.
Direct contact with infected blood may spread malaria, and this can happen via syringe or needle sharing among drug users or through insufficiently sterilized infusion systems. People returning from malaria-endemic regions should not give blood for at least six months.
Symptoms:
Tropical malaria:
It’s the worst kind of malaria, responsible for the deaths of up to 20% of patients who go untreated. After an incubation period of a week to two, flu-like symptoms such as fatigue, headache, aching limbs, and fluctuating temperature become apparent. Anemia, diarrhea, and maybe even central nervous system abnormalities might develop later in the course of the illness. Seizures, amnesia, and coma are all possible complications of the first symptoms.
Tertian malaria:
Malaria tertiana often develops 12–18 days after infection and is characterized by the abrupt onset of a high fever that lasts 3–4 hours and is accompanied by chills and excessive perspiration. Fever flare-ups tend to occur every 48 hours. In most cases, those who get this strain of illness will recover.
Quarterly malaria:
Plasmodium malariae is the causative parasite, and the disease is uncommon. It only affects roughly 1% of cases. Malaria tertiana-like symptoms appear at 72-hour intervals instead of the usual 48. There is an 18 to 40 day gestation period.
Treatment:
Nowadays, a wide variety of powerful antimalarial medications are available. However, the development of resistant pathogen strains raises the possibility of more difficulties.
Prevention:
Since there is no effective active immunization against malaria, the best way to protect yourself from contracting the disease is to avoid being bitten by mosquitoes and to take antimalarial drugs as a kind of chemoprophylaxis. Institutions suggest doing this at least one week before traveling to a malaria-risk region and up to four weeks after returning. The time frame might vary depending on the method used.
Other diseases spread by bloodsuckers
In Europe:
Human granulocytic Ehrlichiosis (HGE)
- Carrier/distribution: Ticks (Ixodes species);
- Pathogen: Ehrlichia sp. (intracellular living bacterium)
- Course: The disease progresses similarly to the flu, with fever, headache, and muscular discomfort; in extreme instances, anemia and brain damage like meningitis may occur. There is a fatality rate of 5%.
- Treatment/prophylaxis: You can take certain antibiotics, but penicillin is not one of them.
Babesiosis
- Carrier/distribution: Ticks (specifically the Ixodes species in Europe), sometimes via blood transfusions; in Europe, the United States, and North Africa.
- Pathogen: In Europe Divergent Babesia (protozoa similar to malaria pathogens)
- Course: Malaria-like symptoms and courses include high fevers, headaches, muscular soreness, weakness, and, in extreme instances, anemia, kidney failure, and spleen abnormalities.
- Treatment/prophylaxis: Antimalarials like clindamycin and quinine are often used.
Mediterranean Spotted Fever (MSF)
- Carrier/distribution: Ticks (genus Rhipicephalus) are responsible for transmission and are found in the region between the Mediterranean and the Black Seas.
- Pathogen: Rickettsia conori (intracellular living bacterium)
- Course: partly local dark skin ulcer, later flu-like symptoms with muscle pain and headache and high fever; 6 percent of cases become seriously ill, in 2 percent MSF is fatal.
- Treatment/prophylaxis: You can take certain antibiotics, but penicillin is not one of them.
Tularemia (rabbit fever)
- Transmission/distribution: Small pockets of infection exist in the Czech Republic, Slovakia, Scandinavia, western Russia, and portions of Austria and are transmitted by direct contact with the blood of infected animals, ticks (Dermacentor, rarely Ixodes), and mosquitoes.
- Pathogen: Francisella tularensis is a pathogenic bacteria
- Course: In cases of bug or tick bite infection, minor flu-like symptoms and fever may follow a period of local skin ulceration and lymph node enlargement.
- Treatment/prophylaxis: antibiotics, partial vaccination
In the tropics
Yellow fever
- Carrier/distribution: The yellow fever mosquito, Aedes aegypti, is the vector and has spread from Africa to South and Central America, with occasional introductions by tourists.
- Pathogen: A member of the flavivirus family of RNA viruses.
- Course: Initially, patients have flu-like symptoms; nevertheless, 15% of them progress to high fever, liver enlargement, and bleeding from internal and external sources. About half of them who have it die.
- Treatment/prophylaxis: Vaccination
Dengue fever
- Carrier/Distribution: The yellow fever mosquito, Aedes aegypti, is responsible for transmission and is found mostly in tropical and subtropical regions, although some instances have been documented in more temperate regions when infected mosquitoes have been intentionally released.
- Pathogen: RNA virus belonging to the flavivirus family
- Course: Dengue fever is characterized by severe fever, chills, and discomfort, and may cause severe hemorrhage and shock in rare instances, especially in children and teenagers.
- Treatment/Prophylaxis: There is no cure or prevention available, just symptomatic treatment.
Sleeping sickness (African trypanosomiasis)
- Carrier/distribution: The Tsetse fly is responsible for transmission; it is only found in tropical Africa.
- Pathogen: Trypanosoma brucei (unicellular flagellates)
- Course: Skin lesions at first, then fever, then infesting internal organs, and finally brain impairment as a final stage. The condition is almost always deadly if not treated.
- Treatment/prophylaxis: Chemical prophylaxis is conceivable, however controversial, and treatment with potent poisons and many adverse effects is available.
Leishmaniasis
- Carrier/distribution: Sand and butterfly mosquitoes (Phlebotomine) are the vectors for this disease, and they may be found in 88 different nations in the tropics and subtropics.
- Pathogen: Leishmania (unicellular flagellates)
- Course: Cutaneous leishmaniasis: at first, there is a stomach ache, followed by diarrhea, and a fever. Changes in blood count and consequent enlargement of the liver and spleen follow. Leishmaniasis is invariably lethal if it is not treated in time.
- Treatment/prophylaxis: Antimony preparations are used for treatment and prevention, although the death rate is still 3–20%.
Bibliography
- Alves SM, Bélo M (August 2002). “Morphometric variations in the housefly, Musca domestica (L.) with latitude”. Genetica. doi:10.1023/a:1020685727460.
- Dahlem GA (2009). “House Fly (Musca domestica)”. Encyclopedia of Insects.
- Dennis DT, Piesman JF (2005). “Overview of tick-borne infections of humans”. ISBN 978-1-55581-238-6.
- Mehlhorn H (2001). Encyclopedic Reference of Parasitology: Biology, Structure, Function. Springer Science & Business Media. ISBN 978-3-540-66819-0.
- Wiegmann, Brian; Yeates, David K. (2012). The Evolutionary Biology of Flies. Columbia University Press. ISBN 978-0-231-50170-5.