Cancer is a terrifying pandemic that hangs over our heads like the sword of Damocles. Innumerable individuals are afflicted by this multifaceted illness, and tens of thousands more must live with the diagnosis every day. Even with the best diagnostic tools and treatment options available, many people still die from it. Doctors are working tirelessly to determine what has triggered this cancerous multiplication of cells.
Some of the possible causes of cancer have been identified as exposure to toxins or radiation or a family history of the illness, although unlike with many infectious diseases, a direct correlation between cause and effect is usually not sufficient for cancer. The catastrophic transition from a healthy body cell to a tumorous cancer cell is often set in motion by the confluence of a number of elements. However, scientists have barely scratched the surface of this interaction’s intricate complexity.
Tumor viruses are one aspect that has gained the attention of scientists. The earliest signs that viruses may cause cancer were identified by scientists around the turn of the past century, but this information was largely disregarded for decades. In the past, there was no link between infectious agents and tumor diseases.
Despite the fact that the link between cancer and viruses was finally proven, scientists in this area faced an unprecedented wall of opposition. Ignorance, but also tenacity, has a long and illustrious history that continues up to the present day. As such, it served as a near-perfect illustration of the typical sequence of scientific progress described by Austrian engineer and author Robert Musil: “Every few years that something till then held to be in error suddenly revolutionizes the field, or that some dim and disdained idea becomes the ruler of a new realm of thought.”
More and more viruses are being added to the list of “suspects” by cancer researchers, and roughly a dozen have been recognized beyond question, demonstrating the “new realm’s” visible growth. The human papillomavirus and various herpes viruses are two examples of these ubiquitous yet purportedly innocuous infections. Viruses’ causal pathways in cancer are very vaguely understood, but researchers are working to fill up the gaps.
The discovery of the cancer virus
Chickens to revolutionize science
In the year 1909, a farmer pays a visit to a young physician and biologist Peyton Rous at his new job at New York’s Rockefeller Institute for Medical Research. He is concealing a jar with a cancerous chicken under his arm. A sarcoma, a huge cancerous tumor of connective tissue, had developed on the right side of the breast of this striped Plymouth Rock chicken.
At the time, research on cancer was still in its infancy, but Rous, who worked on the subject, jumped at the chance to do a battery of experiments using the chick and its tumor. So, he decided to produce an extract from the diseased tissue, filter it to remove any remaining cells, and then inject it into young chickens of the same breed. Unusually for the period, the healthy animals also got cancerous tumors of the same sort as a consequence of this experiment.
With this in mind, Rous deduced that the tumor was caused by a microscopic pathogen present in the extract. He suspected a parasitic creature, probably one of the recently identified viruses. Rous attempted to prove his hypothesis by successfully transmitting additional chicken cancers via this route. His findings and theorization of a cancer-causing virus were published in 1910, setting off a real “tumor wave.”
Standing on the sidelines
However, no success was found in using this method to induce growth in any other animal species. Soon after, Rous was marginalized in the scientific community, and his viral tumors were deemed to be a chicken-specific anomaly. In his acceptance address for the Nobel Prize in 1966, Rous recalled, “The results of the sarcoma virus were met with absolute disbelief.” However, “spontaneous” chicken tumors with different morphologies were successfully transplanted and a virus was found in each of them not long after.
In the 1930s, Richard Shope, a colleague of Rous’s, obtained comparable results using an extract of a benign skin tumor, a papilloma, from the skin of a wild rabbit species. However, these findings were disregarded since they were not thought to be relevant to cancer.
“Milk factor” instead of viruses
The standard medical view, that cancer was at most related to a person’s genes or their environment and could not be caused by viruses or other pathogens, appeared to be impervious to new evidence. Under the banner of “What must not be, cannot be,” any and all theories involving viruses that cause cancer were dismissed as ridiculous. In the 1930s, the United States’ highest health authority convened a council of specialists who issued a formal guiding principle that viruses and other organisms could be ruled out as causes of cancer.
Due to the atmosphere, few scientists were willing to publicly provide proof of the presence of cancer viruses. Breast cancer-causing viruses were first identified in mice by John Bittner, a researcher at the leading cancer research facility in the United States, in the late 1930s. Instead of calling the cancerous agent a virus in his paper, he called it a “milk factor,” neutrally avoiding the risk of losing his job and future research funding.
The breakthrough
The significant change, and the subsequent rise of cancer virus researchers, did not come until the late 1950s. There were two primary causes that resulted in this change: Scientists found that some viruses could introduce their genetic material into the host cell’s DNA. This modified the cells irreversibly without killing them. However, numerous scientists started to find tumor viruses in their lab tests, making it impossible to deny the undesirable reality.
According to a long-held theory, cancer and infections produced by viruses or other organisms could not be linked to one another. But a decade later, in 1966, Peyton Rous was honored for his foresight and tenacity with the Nobel Prize in Medicine, and the virus he discovered was given the honorific name “Rous sarcoma virus.“
Looking for the virus-cancer mechanism
Genome thieves
Cancer cells are the progenitors of more cancer cells and pass on their destructive capacity to their children, making them the ultimate misfits. Yet they originate in healthy tissue. But, how? What part do viruses and other pathogens play in this process? Caltech cancer researcher Renato Dulbecco was pondering this very subject. As a result of Peyton Rous’s rehabilitation, study into tumor viruses is no longer taboo, although still very little is known about how they work.
In 1960, he and his colleague Marguerite Vogt undertook laboratory experiments in which they infected hamster cells with a polyoma virus, a DNA virus with little complexity. The cells started to transform as expected, and tumors started to form. However, they immediately noticed something peculiar: the viral reproduction ceased along with the transition to cancer cells. Their numbers did not increase or decrease as they would during an actual infection since they were not able to exhaust the cell’s resources on viral production. Sure, but why?
The virus always leaves behind traces
Dulbecco could only think of two possibilities: either the virus got killed out in the process of the cell’s metamorphosis, or it survived the transformation but was unable to multiply. After much effort and testing, the scientist finally got an answer. He discovered the virus’s “footprints” in the changed cells, disproving the original hypothesis and confirming the infection was still there.
Using molecular biology techniques, he was also able to show that the virus was inactive since a key piece of its DNA had been incorporated into the host cell’s genome, rendering it inaccessible for viral replication. Only around seven proteins were encoded by the viral DNA that was added, but that seemed to be enough for cell processes to go haywire.
Contrary to dogma
A young scientist at the University of Wisconsin named Howard Temin had less luck than Dulbecco did when he published his findings and received both praise and criticism for them. Unlike Dulbecco, Temin studied an RNA virus (the Rous sarcoma virus) in his tests; yet, he reached the same conclusion as Dulbecco in a 1964 paper: the virus must add something to the cell’s genome that initiates the cell alterations. According to him, before inserting its genetic material into cellular DNA, the virus was “translating” its RNA genome into DNA, called the “provirus.”
However, he made a huge “error” by proposing this theory, since it challenged the prevailing paradigm in molecular biology at the time. This dogma states that information in live cells always flows from DNA to RNA and then to protein, but never the other way around. For this reason, most of Temin’s scientific peers would have considered his concept of a provirus that employed this “wrong” path to be heretical. The response was just as furious and condescending.
Again, it took almost a decade and the “administrative aid” of a coworker before the previously disgraced scientist was vindicated. Temin and the biologist David Baltimore delivered the killing blow to the doctrine at the decade’s close in the 1970s. Both separately found an enzyme in tumor virus-infected cells that can convert RNA to DNA. There was experimental proof that this “provirus DNA” was integrated into the cellular genome.
The seminal work on the biology of tumor viruses by Dulbecco, Temin, and Baltimore was recognized with the Nobel Prize in 1975. However, the three of them were unable to resolve the lingering mysteries of how viruses cause cancer and whether or not they also cause cancer in humans. “I do not believe that infectious viruses are the causes of most human tumors, but I think that viruses can provide us with models for the development of cancer,” Temin said cautiously in his Nobel Prize acceptance address.
Looking for a cancer gene
Can cancer viruses replicate without causing disease?
Two researchers at the U.S. National Cancer Institute, Robert Huebner and George Todaro, experimented with the Rous virus on various mammals in the 1970s, shocking the scientific community just as they were coming to terms with the discovery that cancer viruses, including and especially RNA viruses, incorporated part of their genetic information into the DNA of the cell. They found, to their shock, that viral DNA could be detected in tumor cells even when the tumors had not been caused by the virus but rather by physical or chemical effects. How could this be explained?
The “virogen-oncogene hypothesis”
Huebner and Todaro proposed that viral DNA doesn’t come “out of nowhere” since cells must already have viral genes embedded in their genetic material, which were incorporated into the genome at some point during evolution. These conserved DNA regions are inactive under normal conditions but become functional when exposed to certain stimuli, allowing them to produce viral proteins and, in turn, new viruses. However, they postulated that some of these “virogens” also operated as “oncogenes,” causing the development of tumors as well.
Hunting down the tumor gene
If this hypothesis were to hold, then the Rous oncogene must also be present in the cellular DNA of normally developing animals. Michael Bishop and Harold Varmus of the University of California, San Francisco, began a mission to match the genome of the Rous sarcoma virus with chicken DNA for this very aim. But this would be very difficult to do without high-tech equipment like PCR or sequencing devices.
Fortunately, in 1971, a serendipitous discovery by Peter Vogt of the University of Southern California revealed a viral mutant that was capable of replication but seemed to lack the potential to produce malignant tumors. The virus’s genome was 15 percent shorter than average, suggesting that this missing part could include the critical tumor gene(s).
This was the key piece of information that helped Bishop and Varmus solve the case. This allowed them to determine whether or not the “src” gene fragment was present in the cellular DNA of their guinea pigs and, if so, whether or not it functioned as a possible cancer gene. However, scientists were surprised to discover that the virus was present not just in chickens, the primary hosts of the Rous virus, but in birds of every genus and subgenus.
But that wasn’t the end of it; other researchers soon identified src variations in guinea pigs, rabbits, rats, snakes, and even humans. The oncogene postulated by Huebner and Todaro seemed to be found. Bishop and Varmus, though, were not confident in the claims. They were wary about its extraordinarily widespread distribution. The origin of the gene still remained unknown; did this gene really come from the Rous virus?
Oncogenes: a biological enigma
The enemy within
An essential step forward accomplished with the discovery of a cellular proto-oncogene. Not much time had passed, yet scientists had already uncovered over 40 distinct retroviral oncogenes. They speculated that the majority of cells had gene sequences that were homologous to a viral gene known to cause tumors. Tumor viruses and other external factors could contribute to tumor development, but there was also an “internal adversary” that might be just as crucial.
However, more questions were created by the new data than they answered. Among the most crucial, in Varmus’s words, “Did the evolutionary conservation of the src gene indicate its cellular origin? Or could it still be a virus-derived gene that was just better conserved than comparable viral elements?”
Own cell instead of being smuggled in
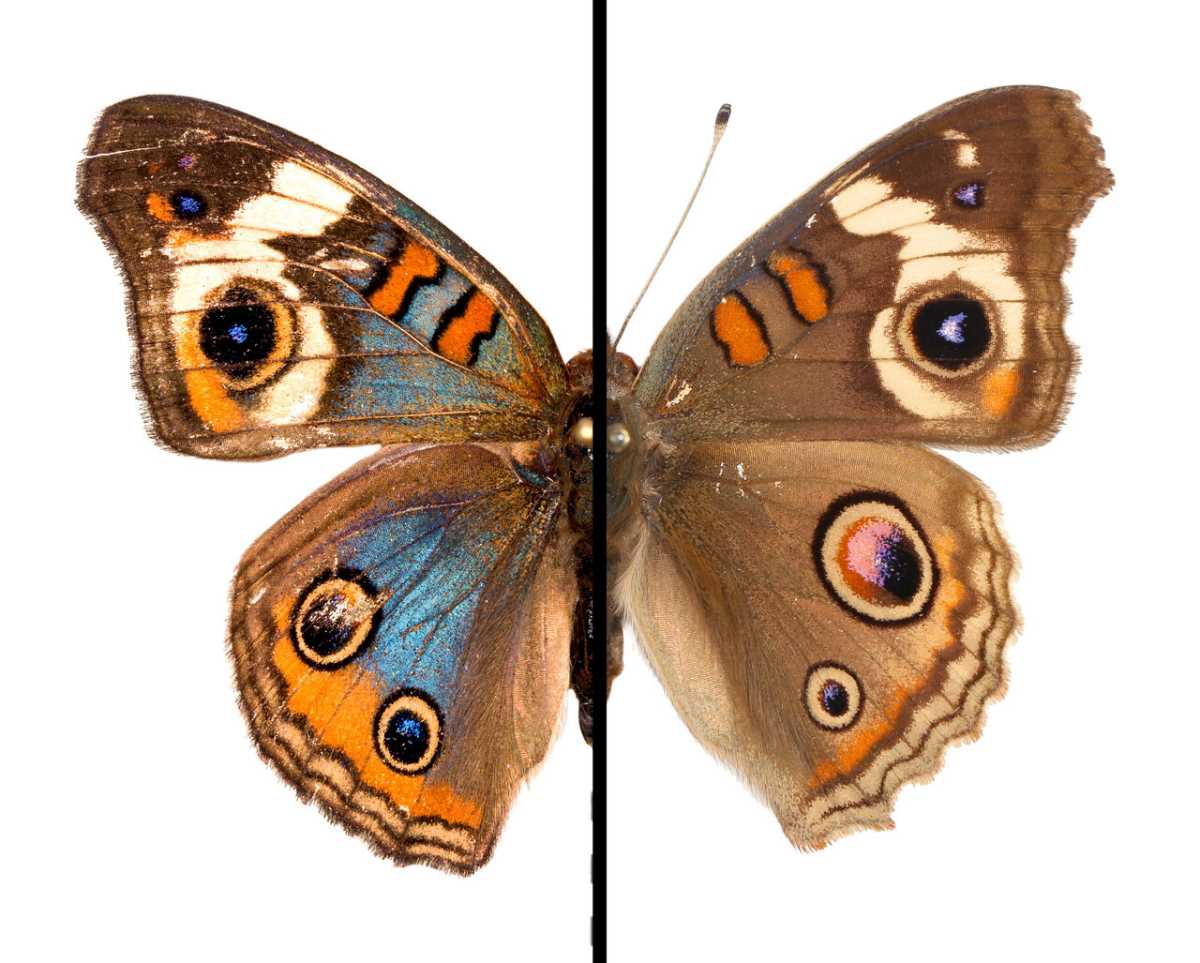
Rapid responses to this question emerged from many different fields. Sequence analysis, however, provided the clinching evidence. It demonstrated that the src gene was broken up into many segments by introns (“junk DNA”), which were typical of biological DNA but were rarely seen in viral genes.
Harold Varmus reflected on this, saying, “All our arguments and experiments led to only one conclusion: the precursor to src was a conserved – and therefore vital – cellular gene that found its way into the Rous sarcoma virus by recombination.” So, it seemed that the proposed evolutionary route of the “virogen oncogene” concept must have followed an exactly opposite direction.
Since the oncogene’s precursors have been conserved throughout evolution, this explained why they are found in so many different types of cells. “Far from being a harmful element just waiting to be activated by a carcinogenic signal, the precursors of viral oncogenes seem to have an impact on the organism to have an important function, otherwise they would not have been preserved in the course of evolution,” said Varmus. These genes are, in fact, involved in essential cellular processes, including multiplication and differentiation.
Hostile takeover
How, therefore, could this normally helpful gene cause an infected cell to go berserk? Bishop and Varmus hypothesized that the retrovirus identifies the benign proto-oncogene during infection and alters it into the malignant oncogene. During this process, known as transduction, the virus inhibits the gene’s regular function and removes it from the organism’s regulatory system. Therefore, the misplaced and overactive genes have undesirable effects, such as excessive cell multiplication.
The two scientists speculated that Huebner and Todaro’s peculiar results might be explained if the transition was triggered by chemical or physical forces. In 1983, researchers found a group of cellular genes that were structurally similar to viral cancer genes and oncogenes from non-viral cancers, lending credence to this theory.
Viruses as a possible cause of human cancer
Initial evidence for human T-virus type 1
By pinpointing the “inner enemy” and showing that viruses might play a role as triggers in carcinogenesis, Bishop and Varmus have thrown open the floodgates for contemporary cancer research. They shared the Nobel Prize in Medicine in 1989.
However, they encountered resistance and even contempt for their ideas. Their hypothesis, that a comparable process could possibly contribute to human tumor formation, was at odds with the current scientific consensus. But this perspective held that although viruses were identified as a cause of tumor disorders in animals, there was less evidence to support a similar link in humans. But they weren’t completely wrong since hereditary or environmental factors are still considered to be the main causes of cancer in humans.
The first human retrovirus
However, this started to change in the early 1980s. In 1980, a patient with cutaneous T-cell lymphoma, a benign skin ulcer, was investigated by virus researcher Robert Gallo and his colleagues at the National Cancer Institute in the United States. He analyzed the tissue samples and found a retrovirus, a kind of virus that had never been seen in humans. While these RNA viruses, to which the Rous sarcoma virus also belongs, had been studied for quite some time in animals, this was the first time that they had been found in people.
Gallo and his Japanese colleagues continued studying its biology and ecology in the years that followed. Scientists found an unexpected link between the virus and adult T-cell leukemia lymphoma; whereas most infected people had relatively mild skin changes over time, a small percentage had acquired this aggressive type of leukemia.
This kind of cancer often does not manifest until the age of 60, but once it does, it generally results in a swift death. It is estimated that just 1–4% of infected people actually acquire leukemia, but all patients carry the virus anyway.
And the Leukemia
So, was the virus the cause of cancer? There had to be more evidence than just finding a virus in a cancer cell. But in 1982, Gallo and his group found the viral “culprit” in the virus’s DNA. Since there was no homolog of the viral gene “tax” in the human cell genome, “tax” could not be considered an oncogene in the traditional sense. But when it was inserted into the cell’s DNA, it activated particular T cell growth factors, leading to the unchecked multiplication characteristic of leukemia. The specifics of this mechanism were, however, still little known.
The pathogen, now known as HTLV-1, or human T-cell leukemia virus, made medical history as the first virus known to cause cancer in humans. This discovery sparked what has become a decades-long effort to identify and characterize additional viruses that might cause human tumors. Even while the hepatitis C pathogen was now thought to have a role in certain kinds of liver cancer and maybe even in some forms of non-lymphoma, Hodgkin’s other RNA viruses had thus far been on the suspect list at best, with nothing yet confirmed.
Human papillomavirus (HPV) and cervical cancer
Forming a model
Human papillomavirus (HPV) is a tiny, contagious virus that may manifest in anyone’s cells. The current global prevalence of this DNA viral infection is estimated to be above 25 million. The sexually transmitted disease affects almost half of the male and female population.
Infected people may not even realize they have it. The virus is asymptomatic and may live in the skin and mucous membranes for a long time; in rare instances, benign warts may appear. In addition to its pervasiveness, HPV is also remarkably diverse, with over 130 distinct strains having been found to date. And 18 of them are particularly worrisome since they belong to high-risk categories and may cause cancer. Discovered in 1983, this link between a virus and cancer is now one of the best studied and proven anywhere. Some virologists think that HPV is responsible for at least 600,000 instances of cancer globally; other estimates place the number at between 12 and 15 percent of all tumor cases.
Two proteins that sneak into cells
The human papillomavirus types 16, and 18, are mostly to blame. More than 90% of head and neck cancers and 99% of cervical cancers have these abnormalities. In most cases, the human immune system can clear up an HPV infection in around ten months. Changes occur, however, when risk factors are introduced, such as smoking, an impaired immune system, or a particularly aggressive viral strain:
Two viral proteins, E6 and E7, are produced by the infected cells. When bound to a particular cell protein, E6 triggers that protein to label the tumor suppressor gene P53 for destruction. Consequently, the cell is deficient in a key component for preventing mutations and cancerous transformations. Another viral protein, E7, is responsible for cell death by “hijacking” a cellular protein engaged in crucial regulatory mechanisms. This causes the release of transcription factors that actively promote cell multiplication. Two proteins assist the virus in disrupting the cell’s basic metabolic and developmental processes, leaving the cell vulnerable to mutations.
However, this is by no means the sole mechanism by which HPV causes cervical cancer. In fact, new mechanisms are disclosed virtually every week. These two, though, are the sharpest and most consequential.
The dirty dozen
Researchers have had a hard time finding new tumor-inducing viruses due to the intricacy and variety of the processes and regulatory systems already engaged. This is one of the reasons why just a handful of anti-cancer drugs that target viruses have been shown to be effective in people.
Epstein-Barr virus (EBV) for nasopharyngeal cancer and Hodgkin’s lymphoma; hepatitis viruses B and C for liver cancer; human T-cell lymphotropic virus type 1 (HTLV-1) for cervical cancer; and human herpesvirus 8 (HHV-8) as a trigger for Kaposi’s sarcoma are all well-established viruses that cause cancer in humans. Polyomavirus and hepatitis C for non-Hodgkin’s lymphoma, and an unidentified agent for a kind of pediatric leukemia, remain on the list of possible tumor-causing viruses. The tally of cancer viruses in humans that have been “condemned” continues to increase today.
Helicobacter pylori and stomach cancer
Several kinds of cancer in humans now have a known link to infections with certain viruses, bacteria, and parasites. 15–20% of all malignancies are believed to have an infectious cause. But we weren’t always aware of the cancer-causing bacteria. In fact, this medical dogma was toppled anew by a dogged scientist, a little bit of self-experimentation, and a giant leap forward. The Australian scientist Barry Marshall, his colleague Robin Warren, and the rod-shaped bacteria Helicobacter pylori are the story’s primary characters.
In 1982, the medical community accepted the dictum that “Bacteria are everywhere—but the human stomach is bacteria-free.” Because of the very acidic conditions present in the stomach, it was often believed that no bacteria could thrive there. And that was not all. The majority of medical professionals and scientists in the field of pharmacology, as well as patients, attributed the pain of gastric mucosal inflammation and subsequent gastric ulcers to the presence of acid in the stomach. The pharmaceutical industry promoted acid blockers of different sorts with the slogan “No acid, no ulcer,” and sales were booming as a result.
Its home is the stomach
Pathologist Robin Warren found something that shouldn’t be there when he examined tissue samples from stomach ulcers and irritated stomach mucosa under a microscope: bacteria that are full of mucus. And that was the case in over half of the samples he tested. The number of these cells seemed to be correlated with the degree of inflammation. Warren consulted with doctor Barry Marshall after concluding that his finding must be significant.
As a team, they achieved the first successful cultivation of the bacteria. They could now undertake microbiological experiments to learn how the bacteria manage to thrive despite the harsh circumstances of the stomach. To begin attaching to the mucosal cells, bacteria first use their flagella to dig deeply through the protective mucus layer. Meanwhile, they used an enzyme called urease to convert the uric acid produced by the cells into carbon dioxide and ammonia. This created a neutral environment that bypassed the stomach’s defense against microbes.
A sip alters the course of history
However, these results did not establish beyond a reasonable doubt that this particular bacteria caused an inflammation or cancerous tumor. Because the conclusive evidence was still absent. In July of 1984, after months of testing, Marshall decided to take a daring step: he began testing on himself. On the informal principle of “a small sip for a person-a big sip for medicine,” he consumed a brackish solution containing billions of germs. As Marshall reflected, “Everyone said, you’re crazy. It seemed like too incredible an explanation for something as complex as stomach ulcers.”
In a matter of days, he started feeling sick, like he had the flu, and in two weeks, he had gastritis. With the use of a tissue sample, he was able to see that his mucosal cells were covered in a thick layer of germs. Thus, Marshall successfully exposed Helicobacter as the true culprit in the inflammatory process. At that time, though, the link he suggested between the bacteria and stomach cancer had not been proven.
The murderer’s in the blood
However, since then, his theory has been independently verified: antibodies may indeed identify the bacteria in the blood. Three further significant epidemiological investigations followed this. Scientists looked for Helicobacter antibodies in the blood of thousands of stomach cancer patients, whose blood was collected and preserved decades ago as part of earlier research, and compared the findings to the values of a similarly large sample of patients who did not have cancer of the stomach.
Those who were infected with Helicobacter 20 years ago had a six-fold increased risk of developing cancer compared to those who were now free of Helicobacter. These findings were so compelling that in 1994, the World Health Organization’s International Agency for Research on Cancer (IARC) officially labeled Helicobacter pylori a class 1 carcinogen, the first identified bacteria capable of causing cancer.
Terms related to viruses, cancer, and genes
Most of what we know about how genes play a role in cancer was uncovered via studies of tumor viruses. The relative simplicity of the viral genome has been the only thing that has allowed researchers to identify, or at least narrow down the DNA building blocks involved in the formation of human cancer.
The link between viruses and cancer has been recognized to exist in animals since the middle of the past century, but only in people since the 1980s. Unlike animal tumor viruses, however, the link between human cancer viruses and the disease is based on correlations or presumed processes rather than a clear cause-and-effect premise. The viruses have a role as either cofactors or cocarcinogens in this scenario. This demonstrates undeniably that the process of carcinogenesis in humans is intricate and multi-staged.
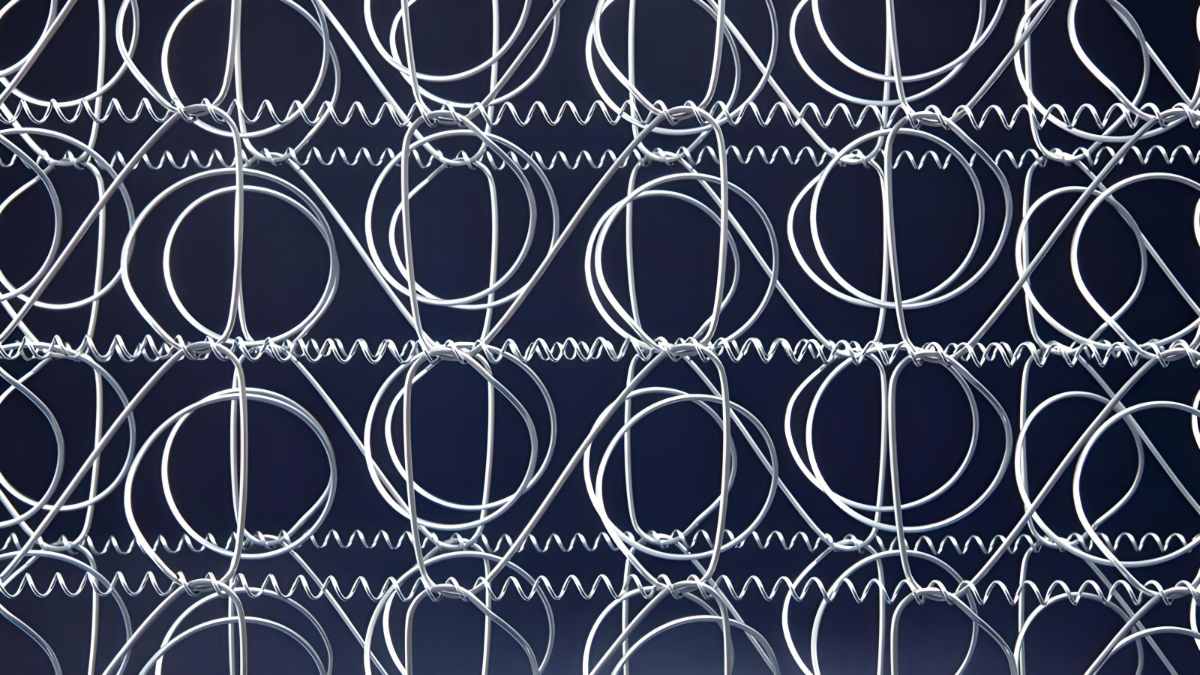
At least six families of DNA viruses and two families of RNA viruses are suspected in the development of cancerous human tumors. Among the examples are Retroviridae and Flaviviridae as RNA virus families and Hepadnaviridae, Herpesviridae, and Papillomaviridae as DNA virus families.
RNA viruses:
Those are the viruses that employ RNA rather than DNA to store their genetic information. Single and double-stranded forms of the RNA are possible. Examples of RNA viruses include influenza, polio, and Ebola; the hepatitis C virus has been linked to cancer.
Retroviruses:
The retrovirus family is also an RNA virus. To integrate their genome into the host cell’s chromosome, retroviruses employ the enzyme reverse transcriptase to create a DNA translation of their genome. Here, it is incorporated into the DNA of the cell for good. The AIDS virus and HTLV-1, a virus linked to leukemia, are examples of such pathogens.
DNA viruses:
These viruses have their genetic material in the form of DNA and may thus integrate it into the host cell’s genome without first requiring “translation.” Herpes viruses, human papillomavirus (HPV), linked to cervical cancer, and Epstein-Barr virus, linked to certain types of leukemia, are all examples.
Transduction/transformation:
This is the process through which healthy cells mutate into cancerous ones. This mechanism has been greatly elucidated by the capacity of viruses to convert cells in culture. The altered cells display hallmarks of cancerous tumors, including unchecked multiplication, reduced reliance on supporting tissue, and less need for external growth hormones. When transplanted into a new host organism, some altered cells may potentially become cancerous.
Tumor virus transformation of a cell always exhibits the following three characteristics: it is a “one-hit” process, meaning that the transformation is triggered by a single viral infection of the cell. In addition, the cell retains some viral genetic information, and the transformation is maintained by the continued production of a subset of viral genes.
Oncogene:
A gene that has a significant role in causing or facilitating the progression of cancer. Point mutations, rearrangement of its DNA building blocks, loss of individual segments, and excessive, uncontrolled gene expression triggered by viruses all contribute to its activation and transformation into a tumor gene. The Greek term for “mass” or “lump” is whence we get our modern word “onco.”
Cellular Oncogenes:
An oncogene may mean either a normal gene that has been changed to become active in tumor cells or a cellular gene that has been activated in tumor cells.
Viral Oncogenes:
DNA viruses may cause cancer because they include a gene that isn’t found in cells but has the potential to do so when infected, or because they contain a version of a normal cellular gene that has been changed or activated to operate as a tumor inducer.
Proto-oncogene:
A precursor of both viral and cellular oncogenes, a normal gene of the cell that may be turned into an active oncogene by external factors.
Tumor suppressor gene (TSG):
Genes encoded by a cell’s own DNA inhibit cancerous transformation. These genes may have a bigger effect on carcinogenesis than the active oncogenes.
Bibliography
- Viruses Associated with Human Cancer – PMC (nih.gov)
- Zur Hausen H. “Novel human polyomaviruses – re-emergence of a well known virus family as possible human carcinogens”. International Journal of Cancer.
- Woolhouse M, Scott F, Hudson Z, Howey R, Chase-Topping M (2012). “Human viruses: discovery and emergence”. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences.
- Koonin EV, Senkevich TG, Dolja VV. “The ancient Virus World and evolution of cells”. Biology Direct. doi:10.1186/1745-6150-1-29.
- “Virus Taxonomy: 2021 Release”. talk.ictvonline.org. International Committee on Taxonomy of Viruses.
- Breitbart M, Rohwer F. “Here a virus, there a virus, everywhere the same virus?”. Trends in Microbiology. doi:10.1016/j.tim.2005.04.003.